Exercise therapy: the treatment of choice
This months blog has a focus on exercise for knee osteo-arthritis (OA), an issue that I’ve had a passion for treating for many years.
It’s predicted that arthritis will soon impact over 3 million Australians.
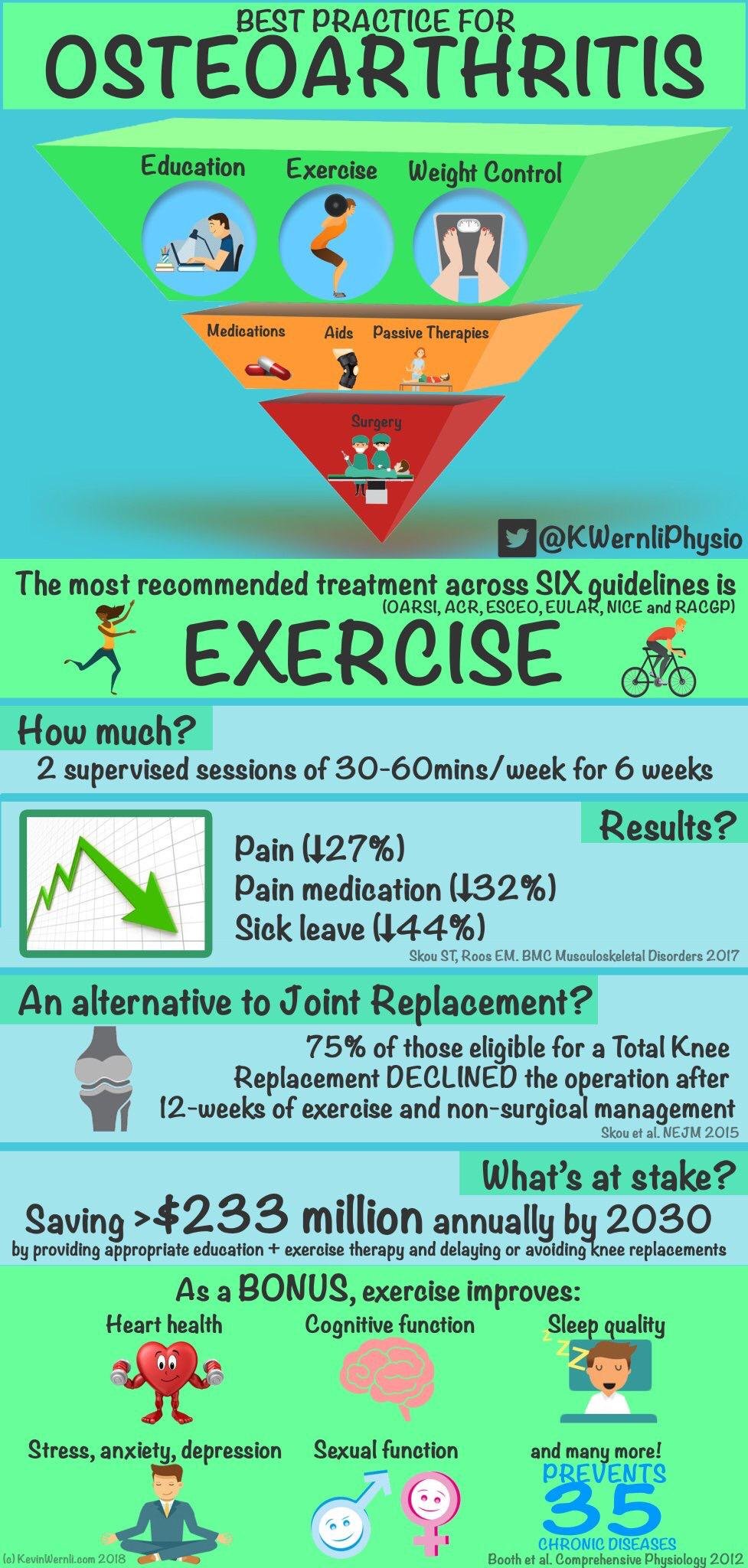
Thankfully, there has been some very positive research showing the benefits of combining a tailored Physiotherapy program with an exercise program to build your bodies capacity, with significant benefits in the short term (six weeks) and long-term (one year).
I hope you will find some useful information and if you know anyone suffering with knee pain from OA, it would be great if you could please share it with them.
Current guidelines recommend exercise for everyone with knee osteoarthritis, irrespective of radiographic disease severity.
Evidence shows a personalised exercise program, gives the best long term outcomes.
These exercise programs consist of:
specific neuro-muscular exercises to help align the knee joint
cardiovascular aerobic fitness
strength training
Ideally this exercise program is set up by a Physiotherapist after a comprehensive assessment.
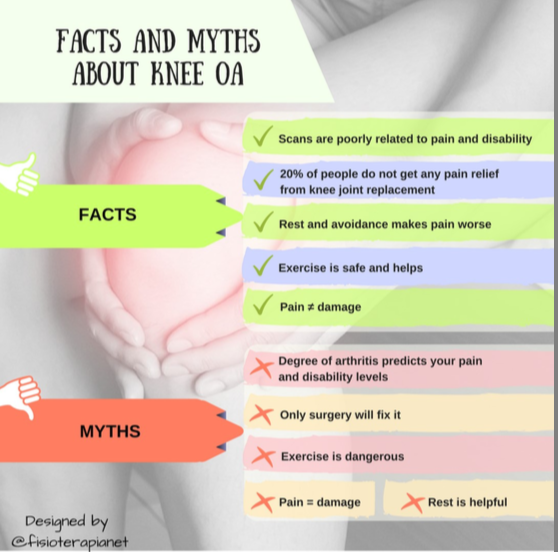
Is exercise and movement safe for people with knee OA?
It is a common misconception that exercise causes arthritis.
Research shows that the main risk factors for knee OA are:
excess body weight
reduced muscle strength
knee mis-alignment
history of a prior traumatic knee injury
An important point to make here is that (except for traumatic injury) all of these factors are modifiable, meaning we have control over them.
This can be quite an empowering feeling, when you contrast this with someone who is told by a specialist, after viewing their scans, that nothing can be done, apart from surgery.
The risk of pain and injury are greatest when your physical capacity is low, as it sets you up for constant overload and damage.
It's important to note that regular moderate exercise strengthens joints and can decrease the risk of osteoarthritis.
Moderate activity levels provide the ‘sweet spot’ for physical health and acts like a vaccine against injury.
Getting past the fear of movement in OA
APA physiotherapist Dr Christian Barton, an OA researcher at LaTrobe University, says:
“One of the biggest problems we have to address is that many people are told to rest when they have pain, rather than stay active. As a result they often become quite sedentary, which can lead to depression, weight gain and an increased risk of other chronic diseases.
Proper exercises, regular physical activity and good health education are essential for OA management, all of which can be delivered by exercise specialists like physios. The missing link is the funding to provide patients the opportunity to do this.”
You Have Two Options:
OA Diagnosis —> Fear of doing more damage —> rest/avoid activity —> deconditioning —> depression —> weight gain —> increase load on knee —> downward spiral —> general health declines
OA Diagnosis —> Consult with Physiotherapist (with a special interest in knee OA) —> personal assessment —> address fear of movement —> set up with graduated exercise program —> Physiotherapy manual techniques to decrease pain, improve joint alignment —> re-build capacity —> maintain happy and healthy life
What is the point in doing exercise and rehab if I’m eventually going to need surgery?
The first thing to keep in mind is that not everyone with OA will progress to a point where they need a joint replacement.
In fact only about 30% in those are diagnosed with OA subsequently go onto require a total knee replacement.
We know that ‘prehab’ gives significantly better outcomes if you do eventually need to go for surgery, so by getting your knee stronger and more robust will have direct benefits. You
A Few Notes On Pain
As you start to move more, you most likely feel some knee pain.
It's critical though you understand one key fact: "Pain does not equal tissue damage".
The truth is pain is related to the threat of tissue damage, not actual tissue damage.
There is a whole field of pain neuroscience research now showing that the pain you feel is not correlated with how much tissue damage there is.
This is relevant to know for people with knee OA, as many people have severe joint degeneration on x-rays, yet have absolutely no pain.
Rather pain is a 'request for change' and in chronic knee pain may be more related to ongoing weakness and stiffness in the knee.
A sure sign that movement is needed to get the muscles stronger and protect the knee joint.
It’s OK for exercise to be painful (especially as you warm-up at the beginning), but try and keep it to an acceptable level (e.g. < 5/10). Also, monitor the response in the following 24 hours after you exercise.
Patience is key.
As you build your capacity over time, you will get less intense and frequent pain flare-ups.
Credit: Christian Barton Presentation
Three Components To An Effective Exercise Program:
Neuro-muscular control
One important risk factor that can lead to progression of knee OA is the mis-alignment of your knee (in particular the kneecap).
Many people with knee pain who get motivated to exercise may end of causing a flare-up if there knee is out of alignment.
Some signs you may have a knee alignment issue:
general ache/pain in the front of the knee
pain aggravated activity involving a bent knee and body weight on the leg (e.g. walking up and down stairs, squatting, kneeling, jumping or hopping)
pain aggravated by sitting for prolonged periods e.g. driving or sitting in a movie theatre (eg, jumping, hopping, running, going up or down stairs, or squatting).
some people also hear and feel a grinding / clicking around the knee with mild swelling
A number of factors can alter the mechanics of the patellofemoral joint and increase joint stress, leading to OA.
This is where an detailed Movement Assessment with an experienced Physiotherapist can really pay dividends.
We can quickly see which parts of your body are moving efficiently and which are not and then take the time to out together a customised plan of attack for you and this can have the capacity to not only reduce symptoms but have the potential to slow disease progression.
Manual therapy, dry needling, exercise and taping can all greatly assist with re-aligning your knee joint.
Pilates can also very beneficial it helping to build the neural pathways for efficient movement.
2. Aerobic fitness
Aerobic exercise has many benefits for people with arthritis that include:
stimulating natural endorphins that can help decrease pain as much as taking medications (without the side effects)
builds your physical capacity and increases muscle strength to help protect the joint
helps in managing your weight (there is a large body of evidence that identifies obesity as a risk factor for developing OA of the knee, particularly in women)
improves mental health and lowers the risk of depression and anxiety
getting you out of the house and away from sedentary behaviours
strengthens social connections
What exactly is aerobic exercise?
Aerobic exercise can be defined by light to moderate intensity, and is characterised by our ability to maintain it for a prolonged duration (many minutes to several hours). You should be able to maintain a conversation as you move.
Capacity vs Demand
We know that your symptoms are likely to flare-up when you get fatigued. It is important to build your cardio-vascular capacity so you can comfortably perform your everyday activities with ease and comfort.
When you’re had a flare-up and are in pain, your activity levels tend to drop off. This has in impact on your bodies capacity, and your ability to deal with demand and loads will be temporarily reduced, until you can build it back up again.
Pacing yourself with a graded exercise program is the best way to re-build capacity. Monitoring your time, distance and pace can be extremely beneficial with a GPS watch or app in your phone.
How much aerobic exercise should I aim for?
Current guidelines recommend aerobic exercise be performed ideally on most, and preferably all, days of the week, for a minimum of 30-60 minutes a day.
This 30-minute total can be performed in one go, or be made up of 3 x 10-minute sessions, if that’s more convenient for your lifestyle.
How do you choose what sort of cardiovascular exercise to do?
“The best exercise is the one you’ll commit to doing”
Factors to consider:
What do you enjoy doing and what you will commit to?
How much time do you have to fit into the day?
Do you have any social support that would increase adherence?
Before you begin
As you begin an exercise program, you may need to allow a period of 'body tuning' i.e. using manual therapy, massage, dry needling and specific exercises to improve tissue quality and joint alignment.
Similar to playing an instrument, tuning up before hand makes things perform much better and reduces the wear and tear.
Walking
Gradually increasing the amount you walk would be an excellent way to start building your aerobic fitness.
Don’t forget to invest in some good quality shoes that are replaced every 3-6 months, depending on how active you are.
Cycling
While cycling can be good for the health of the knee joint, unfortunately it can contribute to muscle imbalances.
Specifically cycling inhibits the glutes and makes the hip flexors and hamstrings tighten up. This can have consequences when walking and standing for long periods, as the knee joint is likely to experience increased load and strain.
If you really enjoy cycling, that’s cool, but you may need to spend some extra time working on correcting your muscle imbalances.
Running
For many years it was thought running ‘caused bad knees’ and it was best to avoid if you have knee pain.
However, much research has come out recently with some surprising findings - runners are at a reduced risk of developing knee arthritis.
The exact mechanisms for this are still unclear, but may be related to runners maintaining a healthier weight level, with stronger muscles and more resilient joints.
BENEFITS OF RECREATIONAL RUNNING - Recreational running is not only good for your overall health, but also benefits your knees and hips—just 3.5% of these runners develop hip or knee arthritis. A sedentary lifestyle—not running—or competing as an elite runner increases the risk of hip or knee arthritis by 10.2% and 13.3%, respectively.
Source: Journal of Orthopeadic Sports Physical Therapy
Bottom line: there are certain strategies for helping offload the knee when running (such as increasing your cadence 5-10%) to keep you from aggravating your knee pain. Please contact us to find out more.
Swimming
Getting in the water regularly would be one of the best things you could do for knee OA. The buoyancy of the water helps decompress the joints and allows you to move freely with minimal pain. Swimming, water aerobics or even just walking in the water can be very healing for the knee joints.
Just ensure you are still getting enough weight bearing exercise to stimulate your muscle and bone growth.
3. Strengthening
National guidelines recommend x 2 strengthening sessions per week.
This doesn’t mean you you need to necessarily go to the gym, (but it may be helpful if you have a small weights at home) to gradually progress your strength capacity.
Your Physio will be able to guide and progress your strength program.
Major muscle groups that should be targeted include the quads, glutes, hamstrings and calves.
Dealing with flare-ups
flare-ups are a natural part of the OA presentation and should be expected
the main thing is to listen to your body and temporarily reduce any load and strain for a few days
focus on non-weight bearing exercise such as pool and pilates exercises to help keep strength in glutes and core
take panadol as needed
use ice or heat packs
keeping an activity log to monitor how your body responds to your exercise can help identify triggers
If your symptoms persist for more than a few days, make an appointment to see your Physio.
How can a Physiotherapist assist someone with knee OA?
1. Assessment and Diagnosis
A modest investment in a Physio Assessment early on in your journey pays big dividends in terms of identifying relevant contributing factors and helping you get on the fast track to healing.
We spend a lot of time in the beginning educating you so you know what to expect in terms of recovery and what you need to do, to manage your recovery successfully.
"Give me six hours to chop down a tree and I will spend the first four sharpening the axe." - Abraham Lincoln
2. Dry Needling / Massage and Taping
Often 4-6 sessions of manual therapy will help minimize pain, re-set your tissues and get you into a position where you can confidently self-manage.
Muscles that are commonly tight and affecting your knee include the
ITB
TFL
hamstrings,
quads and calves
Foam rolling and spiky ball massage are effective at maintaining flexibility, but dry needling has the ability to get to the deeper part of the muscle and get a more effective release.
Find out more about dry needling here.
We can also show you how to tape your knee to provide relief in the short-term.
3. Guidance on load management
We will give you advice on how to gradually re-load your tissues to safely protect your knee from future flare-ups. We work with your coach or trainer to manage your return to doing what you love.
4. Building a personalised home exercise program
You are the most important part of the healing process and what you do is the most important part getting you better.
We use the convenient Physitrack App to build your personalised home program with videos delivered to your smart phone.
5. Movement Re-Training
Once your pain is under control we then watch how you move and optimise your movement patterning to decrease the chances of the knee pain returning.
Pilates can be a very effective way to maintain efficient movement patterns.
Is Knee Pain or Injury keeping you from being as active and healthy as you want?
Summary
I hope this post has given you some valuable guidance in planning your exercise to help your knee. It is very general information, so please consult your Physiotherapist for advice specific for you.
There is a lot of positive research now that shows taking a proactive approach to your health can have a very successful outcome for your knee pain.
If you have knee issues and like some more personalised guidance, it would be a pleasure to help you (we can help in person or via our online tele-health portal).
Please take a moment to fill out the form below and we’ll get back to you as soon as possible.
Knee OA - Part 2 - Exercise
1. Do you think exercise is a beneficial intervention for knee OA patients. If so why?
Yes exercise is very beneficial for knee OA.
2. How often do you prescribe exercises for knee OA patients?
Doing some form o
3. What are the most effective exercises for your pt groups.
For knee pa
4. Do you often see changes in patient function and pain after an exercises prescription? If so what sort of changes do you often observe?
5. How many days a week should OA patients exercise?
6. How many repetitions and sets do you often prescribe patients with mild, mod and severe knee OA
7. How many times a week do you often prescribe such exercises?
8. What sorts of lower limb exercises do you prescribe patients with knee OA and why?
-