The Best Defence Is A Good Offence
If you've had a few niggles or been in pain recently, you might find yourself feeling a little overwhelmed. Sometimes the pain forces us into a defensive or protective mode.
Defensive strategies could include:
- ignoring the pain & hoping it will go away
- regularly taking pain killers / anti-inflammatory to numb the pain
- reducing or eliminating any sort of exercise for fear of causing a flare up
You may also find yourself bracing your body rigidly, every time you move or you may hold your breath (subconsciously) the majority of the time.
Defence IS an important short-term strategy for a new injury, don't get me wrong.
But, after a few months, you're tissues have generally healed the best they can.
Then you've got to take a leap of faith and breakout out of defence and start to re-build proactively...step by step.
When planning your offensive play...success comes from having multiple strategies.
Just like in sport, if you're repeating the same offensive strategy all the time, your body will quickly see it coming and the positive adaptations become limited (and the risk of overuse injuries increases).
The best offence to build resilience in your body would include a good variety of types of movement.
Forming the foundation would be doing a form of Cardio aerobic exercise (whatever you enjoy), Pilates, Yoga, strengthening with a PT, and weight bearing exercise to stimulate bone growth.
Challenge for 2018:
Try x 5 NEW types of exercise or movement approaches that you haven't tried before.
TIP: try something that is the opposite of what you currently do. If you tend towards high intensity exercise than try something easier. If you tend to do easy stuff try something more intense.
Some movement options you could try:
- hiking, stand up paddle boarding, rock climbing, triathlon, cross fit, F45, orange theory fitness, Feldenkrais, karate, surfing, dancing, Parkour, BOUNCE, acroyoga, foam rolling, restorative Yoga, sprinting, 7 min workout, mountain biking, tennis, Aussie rules (especially for women!)
Keep challenging yourself.
Your body and mind will thank-you :-)
Runner's Knee
Patelleo-Femoral Pain Syndrome / Runner's Knee Treatment in Adelaide
The Resilient Knee Project is an innovative solution for people with chronic knee pain that empowers individuals to self-manage their pain and most importantly, get them back to enjoy the physical and mental benefits of running.
Founded by Daniel O’Grady, dedicated professional with first hand experience of overcoming knee pain and running the NYC Marathon, the project aims to be a world leader in restoring people’s confidence in their knees and get back to doing what they love.
Is The Resilient Knee Program right for you?
Start a conversation with our new Chat Bot HERE
What is Runners Knee (Patellofemoral Pain PFP)?
Patellofemoral pain (PFP) is a common condition where pain is felt on the front of the knee, either around or behind the patella.
It occurs in up to 20% of the population (1).
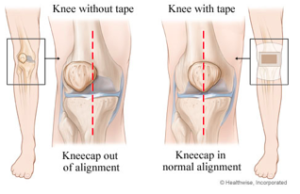
The patellofemoral joint is made of the kneecap (patella) sitting on the front of the thigh bone.
The patellofemoral joint functions as a pulley system to help the quadriceps muscles straighten the knee most efficiently.
There are around 20 muscles that hold the patella centred and aligned.
Pain often results when there is excessive compression on the patella or a muscle imbalance around the patella causes misalignment of the patella.
Over time, this causes rubbing of the joint surfaces, creating inflammation and pain.
What are the most common symptoms of PFP?
general ache/pain in the front of the knee
pain aggravated activity involving a bent knee and body weight on the leg (e.g. walking up and down stairs, squatting, kneeling, jumping or hopping)
pain aggravated by sitting for prolonged periods e.g. driving or sitting in a movie theatre.
some people also hear and feel a grinding / clicking around the knee with mild swelling
An x-ray or MRI is not usually necessary to diagnose PFP.
Patello-femoral pain is often mis-diagnosed as knee osteo-arthritis in young people, due to the deep ache that is often felt.
An assessment by a Physiotherapist will help to clarify your diagnosis.
Who is most likely to be affected by PFP?
The main risk factor for developing PFP is recent spike in training load.
PFP is common in:
runners
cyclists
triathletes
cross fitters
football, basketball, jumping sports
hikers (especially going downhill)
Biomechanical issues that can predispose to PFP include:
weakness in glutes, quads (VMO), core, calves
tight ITB, TFL, quads (outer), hamstrings, calves
stiffness in ankles (e.g. post ankle sprain)
stiffness in the hip joints / hip flexors
runners with who predominantly heel strike
White et al (2009) showed that patients with patellofemoral pain had shorter hamstring muscles than asymptomatic controls.
What is the most effective treatment?
There is strong evidence to support a tailored physiotherapy (including exercise, education, taping), compared to placebo in the short (six weeks) and long-term (one year).
Evidence shows a personalised exercise program (combination of stretching and strengthening) gives the best long term outcomes.
Ideally this exercise program is set up by a Physiotherapist after a comprehensive assessment.
How long until I feel better?
As our understanding has grown, it has become clear that PFP is not necessarily something that will disappear on its own, and some people can have episodes on and off for many years.
As such, in order to have the best chance of recovering from your PFP and reducing the likelihood of it recurring, it is important to understand your condition, your individual contributing factors and what you can do.
For many people, a program of ongoing and progressive exercise (as prescribed by your physiotherapist) is necessary to build and maintain muscle strength, and good movement coordination.
Additionally, there is evidence suggesting that people with PFP may have an increased risk of going on to develop patellofemoral osteoarthritis (OA). Therefore, seeing an experienced physiotherapist for a management program will help you keep your patellofemoral joints functioning as well as possible, and keep you as active as you’d like to be now and into the future.
What can I do?
avoid aggravating activities
ice your knee to eliminate the inflammation (15 mins x 2 day for 2 weeks)
home exercises - foam rolling (see below) and strengthening
For Runners:
avoid hills
cut back on your running mileage
increase your cadence by 5-10%
check your shoes - time for a new pair?
focus on cross training - swimming, pilates, yoga e.t.c.
Some of the common foam roller exercises we prescribe:
Calf
Hamstring
ITB
Quads
How can a Physiotherapist assist with recovery?
1. Assessment and Diagnosis
A Physio Assessment early on in your journey pays big dividends in terms of identifying relevant contributing factors and helping you get on the fast track to healing.
We spend a lot of time in the beginning educating you so you know what to expect in terms of recovery and what you need to do, to manage your recovery successfully.
2. Dry Needling / Massage and Taping
Generally a short burst of targeted hands manual therapy over 3-4 sessions will help re-set your tissues, balance the muscles around the knee and get you into a position where you can confidently self-manage.
Muscles that are commonly tight and affecting your knee include:
ITB
TFL
hamstrings
quads and calves
Foam rolling and spiky ball massage are effective at maintaining flexibility, but dry needling has the ability to get to the deeper part of the muscle and get a more effective release.
Find out more about dry needling here.
We can also show you how to tape your knee to provide relief in the short-term.
3. Guidance on load management
We will give you advice on how to gradually re-load your tissues to safely protect your knee from future flare-ups. We work with your coach or trainer to manage your return to doing what you love.
4. Building a personalised home exercise program
You are the most important part of the healing process and what you do is the most important part getting you better.
We use the convenient Physitrack App to build your personalised home program with videos delivered to your smart phone.
5. Movement Re-Training
Once your pain is under control we then watch how you move and optimise your movement patterning to decrease the chances of the knee pain returning.
People with patello-femoral pain are often hip flexor and quadricep dominant and need to learn how to activate the glutes and hamstrings.
We have some specific exercises to show you to help you fast track this process.
Is Knee Pain or Injury keeping you from being as active and healthy as you want?
Don't delay your treatment...
The occasional ache or pain may be nothing to worry about, but failing to pay attention to strong pain may end up causing you a lot of problems in the future. If knee pain is reducing your ability to take part in the activities your normally do, then it is time to get it looked at. In general, chronic knee pain or clicking that is affecting your life is a sign that something is wrong.
A serious problem will not correct itself, and left untreated, can result in more pain and irreversible damage.
Bookings:
If you think we are the right fit for you and you wish to get relief right away, use our simple online booking system to make an appointment. If you would prefer to speak to us directly, call us 1300 657 813
References:
1. Boling M, Padua D, Marshall S, et al. Gender differ- ences in the incidence and prevalence of patellofe- moral pain syndrome. Scand J Med Sci Sports 2010;20(5):725–30.
2.
Wood L, Muller S, Peat G. The epidemiology of patellofemoral disorders in adulthood: A review of routine general practice morbidity recording. Prim Health Care Res Dev 2011;12(2):157–64.
Dan O'Grady is a results driven qualified Physiotherapist and member of the Australian Physiotherapy Association. Dan has a special interest in treating knee pain. He has been working in private practice for 15 years with (over 20,000 patient consults). He is passionate about helping people to move better, feel better and get back to doing what they love.
Other blogs to help with your knee pain and get your performing at your best:
NYC Marathon In Review
Thursday 2nd November 2017
Up at 3:30am to get on a 6am Qantas flight from Adelaide to Sydney. Thank-you Mum for dropping me at the airport! Flew Adelaide - Sydney - LA - JFK. Sat next to a guy from Sydney who was also running the NYC marathon. It seemed like half the plane was traveling over for the marathon (technically there were 1006 Aussies running).
On the plane, had the chance re-read the George Sheehan classic, 'Running and Being'. Written by a cardiologist, runner and writer his approach to writing and running always inspires.
Landed into JFK and collected my bags. Waiting along side Hawthorn great (now Brisbane Lion) Luke Hodge who was also there to run the marathon. (He did a very decent time of 3:21 by the way).
Friday 3rd November
Had dinner with friends Luke and Marie last night. It was a nice feeling being back in NYC and seeing some familiar faces.
Headed to the expo at the Javits Centre. Was super impressed by the organisation and speed of number pick-up considering how many people were going through.
Adelaide to New York...only a 20 hour plane ride away!
Met a lady who was running the marathon for the fifth time. Her secret was to consume a beer at the 32km mark. She thought that was the absolute key to finishing strong - with a good combo of carbohydrates, electrolytes and alcohol to numb the pain. I will have to try that next time.
After the expo, I headed over to my old gym, the New York Health & Racquet club on 56th street. Ran three kilometers on the treadmill. Ran a couple of kilometers on the treadmill and then went for a swim, stretch and massage on the foam roller. Unwinding the residual tightness from the flight.
A quick lunch at Starbucks and then headed over to Central Park to hear Dean Karinazes speak about his ultra-marathons. His main advice for the marathon - take it easy in the first half and come home strong.
Saturday 4th November
Went to the NYRR in the morning to hear the world champion runners speak and about their careers and NYC marathon strategy.
Running Royalty...from left Haile Gebrselassie, Paula Radcliffe, Bill Rodgers, German Silva and Ryan Hall
There were many pearls of wisdom, but Paula Radcliffe's advice particularly stood out:
“Run the first third of the marathon with your head, second third with your legs and the final with your heart”
After listening to the runners, I dropped my bag off at Orthology, located a stone's throw from the finish line at Columbus Circle. Had a quick run in Central Park to stretch the legs out one last time.
Then spent the afternoon with the feet up and watching the running documentary, Breaking 2.
Inspirational watching these guys run and put everything on the line. I won't wreck the ending if you haven't already seen it, but just to say, if you haven't yet seen it, please do.
Cooked up some pasta for dinner and tried to have an early night.
Race Day - Sunday 5th November
Didn't sleep too well, as you'd expect. Woke at 2am and didn't really get back to sleep. Got up at 4:45am and had a quick breakfast of toast and cereal and then walked over to the 72nd St subway station to get the 1 train down to South Ferry.
Got on board the 6:30am ferry to Staten Island and then a bus over to the start line.
Passed the first test - getting over to Staten Island in one piece. Even had time for half a bagel and cup of tea
I was in wave 2 that started at 10:15am, so I had a few minutes to do some final preparation - ensuring my laces were down up properly, taping my knees, doing a few hip openers, applying some sunscreen and preparing my gels and snacks in my flip belt for easy access.
A few deep breaths and then we were called up to the start line.
This is the moment of truth and before every race I always feel a lot of gratitude, just to make it to the starting line. It's a nice chance to reflect on your journey, the many small battles won and the abundant learning experiences training for a marathon provides. And most importantly, very grateful to all of the people that helped me along the way.
The weather was close to perfect - about 14 degrees with heavy cloud cover and a few light showers in the forecast, although I would have liked it a little colder.
I decided to run with the 3:40 pacer and that allowed me to run on top of the Verrazano-Narrows bridge. After the gun went off to signal the start, we hear Frank Sinatra's song New York, New York playing out across the bridge.
My goal during the race was to stick with the 3:40 group as long as possible. Runners, like cyclists, can benefit from a drafting effect. The person running in front of you buffers you from the wind and you save precious energy. There were probably about 20 people in the group.
As I did most of my long training runs on my own, running in a big group is so much easier psychologically. It is almost like being carried through the streets in a big comfy lounge chair. You just have to be careful of potholes and obstacles on the course that come up quickly due to your lack of peripheral vision.
The best thing about running with a pacer is that they know the course inside out and know when to push and when to take it easy.
Mentally that frees you up big time so you can then pay attention to what's going on in your body. The main metric that I tracked on my GPS watch was cadence. I was trying to maintain 175-180 as much as possible.
When I started feeling a bit tired or sluggish, I noticed my cadence had dropped to 165-170 and by increasing by 5-10% it would immediately ease the pressure on my legs.
It's one of the ironic things about running that I'm still trying to get my head around.
Intuitively, you'd think to run faster you need to step out with a bigger stride. But the opposite is true - higher cadence, turning your legs over more quickly with a forwards lean actually makes you go faster, (with better efficiency).
Running with the pacing group was also beneficial because you didn't have to constantly check times and pace so you could enjoy the spectacle that is the NYC marathon!
For me, the NYC race is all about the people.
The way New Yorkers get behind the marathon is second to none. They 100% have your back on race day. If you are showing even the slightest bit of struggle they will go out of their way to yell your name and put a fire in your belly. The day after the marathon, again many people go out of their way to congratulate you on finishing.
Anyway, back to the race.
The first mile is up and down the Verrazano-Narrows bridge and after that, it's a pretty flat run through Brooklyn and up through Queens.
Things went well early on and I was enjoying the feeling of running and seeing the miles tick by quite quickly and reasonably enjoyably.
At the first 5km checkpoint, I ate a banana and then from there, every 5km a Winners gel (30g of carbohydrate) along with one Allens lolly snake and either a gulp full of water or Gatorade.
At around 12km, I felt the early inklings of some leg cramps, so I downed the salty pickle juice that my nutritionist had recommended. That seemed to help calm the legs over the next 10km.
By the 25km mark I was holding pretty strong as we ran up the Queensborough bridge - the second steepest part of the race. There were lots of people slowing down and feeling the burn...and I was one of them. Managed to lose contact with Paul, the 3:40 pacer.
At the top of the bridge, I was pushing close to my limit and was around 300m behind the pacer.
On the downhill I picked up the pace and latched back onto him as we were greeted with a massively cheering crowd on 1st avenue in Manhattan.
From there, it was a long, straight stretch up to the Bronx. This was a hard part of the race where the reality of running a marathon really kicks in. The race really goes up a notch as the intensity from the crowd ramps up. Trying to keep up with Paul the pacer was tough as I think he picked up the pace a bit too. Thankfully he did the difficult job of weaving around people and making a path and I was close on his heels.
Over the Willis Ave bridge (that connects Manhattan to the Bronx), at about 31km, my legs had enough and I could feel a full blown cramp not too far off. It was mainly in the back of legs in the hamstrings, but the quads weren't too far off either. My legs were pretty cooked after chasing the pacer down the bridge and the glycogen stores were running low. I slowed right down to a walk for about a minute and then once over the bridge and started shuffling again. Thank-fully the walk freshened up the legs and I started feeling better.
In 2015 I also suffered from cramps and so this time, I carried some salt packets, with me. The sodium helps replace the loss from your sweat. I went through the packets pretty quickly and thankfully, the first aid stations were also handing them out and I found these really gave me a few more kilometres of cramp-free running.
Made it through the Bronx and then back over into Harlem and finally made it up 5th Avenue which is long slow uphill. Getting over that and then a few nice downhills in Central Park, although I was slowing right down by then and doing a walk / run combo.
Finally, over to Colombus Circle and up to 67th street Central Park, crossing the finish line in a time of 3:46:50.
Really happy, relieved and actually quite shocked by the time...easily beating my goal of under four hours!
Just after crossing the finish line...
Slow walk up Central Park West
After party at Orthology with Sophia and Jun
Monday 6th November
Walked over to the morning at the Marathon Pavillion, getting my medal engraved and some more foam rolling and stretching out. Then over back over to the NYRR to watch a replay of the marathon. Didn't feel too bad, all things considered. As the day progressed, the delayed onset muscles soreness crept in, in particular the quads...damn subway stairs!
Stretching out in a sea of foam rollers and therabands the day after the marathon. Thanks to the Physios at the Hospital For Special Surgery
My Biggest Struggle
I don't think anyone is every 100% fit before a marathon.
There are always niggles and you try and manage the best way you can.
For me, my left knee was the major concern.
An old football injury nearly 20 years ago resulted in a torn medial meniscus and degeneration. I had an MRI done a few months before the marathon and it didn't look great.
I must admit that deflated me a bit.
Obviously I was wary of any aggravating the pain and potentially causing more damage to the knee. But I also found that the more running I did, the better the knee felt.
What really helped was making a list with two categories - modifiable and non-modifiable contributing factors to knee pain:
Non-modifiable Risk Factors
Structural pathology - damage already down to the mensicus
Genetics
Age
Modifiable Risk Factors
Load management
Running technique
Recovery strategies
Food / diet
Strength / Flexibility
Weight
Movement habits
Accepting that my knee was not 100% and never will be allowed me to focus on ensuring the rest of the foundation was as optimal as possible.
Reflecting back over the past few months, I came up with a few other things that I think helped me achieve my marathon goal:
Philosophy
Capacity vs Demand
Build capacity in a developmental sequence, allowing plenty of time at each stage for adaptation to occur. Running is a high load activity e.g. running 10km is 10,000 steps at 3 x body weight. All that force has to go somewhere.
Recovery
Nutrition advice from Steph Gaskell at Nutrition Strategies in particular ensuring intake of 20g protein x 3-4 spread throughout the day, rather than all at dinner time.
Daily foam roller + tennis ball release (great techniques learnt thanks to Yoga with Jem)
Restorative Yoga with Evelyn at Yogita
Pilates x 1 week
Regular ice baths
Got A Running Coach
Thanks to Sam Hicks who really helped me with strength training and building a road map towards my goal. He had me do some quality runs in the last few weeks before the marathon that really helped prime my body for race day.
More Running, Less Hills
Previously I did too much Mt Lofty. Running up there x 2 week was good for the cardio-vascular fitness at the expense of my hip flexors getting really tight. This time I trained hills x 1 per week but they were short sharp repeats that allowed more time for the longer runs.
Flip belt
This was a life saver - carrying my gels, lollies etc in a comfortable position around my waist. I would recommend you try this in all of your long runs as it took a little bit of getting used to.
Music During The Marathon
In 2015 I wanted to experience the full vibe of NYC and didn't wear head phones.
This time I took my phone and at around the half way point (as soon as I was starting to struggle) put on the NYC playlist.
I found this was a REALLY good way to re-focus.
Even though the crowd is amazing, it's sometimes nice to get back in your own space for a few minutes.
You can check and out my cheesy motivational Playlist here
In Summary
NYC marathon was an incredibly fun and inspiring experience - it's definitely a 'bucket list' thing to do. I can say the process and learning journey building up to the marathon was just as satisfying as the race itself.
If you ever get the opportunity to run the NYC marathon, I'd highly recommend you take it!
Tendinopathy Update
The past weekend I attended Peter Malliaras's course, 'Mastering Lower Limb Tendinopathies'.
Peter is an Associate Professor at Monash University and has spent many years researching and working with people with tendon problems.
In recent years there has been a lot of significant new research in the world of tendon rehab.
If you've ever had an issue with an ongoing tendon problem, you can understand how frustrating the long term pain and dysfunction can be.
There is much conflicting advice and out dated treatment approaches that can contribute to the poor outcomes many people face with tendon injuries.
Thankfully, Peter has put all of the latest based evidence into a comprehensible format and in this blog post I'd like to share just a little summary.
This blog would be particularly helpful if you suffer from ongoing pain in the:
Achilles tendon
Hamstring
Patella tendon
Hip pain/bursitis
Plantar fascia
What is a tendon?
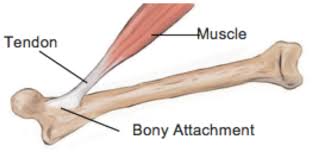
Tendons connect the muscle to bone. They are made up primarily of collagen fibres.
In the lower limb, role of tendon is to absorb and release energy
Tendons are like springs that absorb stretching forces and then release energy when we move.
What causes tendon problems?
Tendons are very sensitive to changes in load.
Essentially, tendons become injured when we over-load them too soon, or when demand exceeds capacity.
This can be from:
too much volume
too much intensity
change in footwear or surface
For example a runner may start to include sprinting or hill work too soon or increase mileage suddenly leading up to a big race.
High training load is not a risk for injuries, it's how you get there that is the important factor (i.e. avoiding acute spikes in training loads).
Tendons become damaged when demand exceeds their capacity
What is the difference between Tendinitis and Tendinopathy?
Tendinitis refers to the inflammation in the early stages of an injury.
This is opposed to tendinopathy that refers to the process of degeneration that tendon goes through in response to chronic overload.
Recent research suggests a lot of what we previously thought of as tendon inflammation was actually related to tendinopathy.
Who is likely to suffer from a tendon problem?
Patella tendon (front of knee)
Usually occurs in younger people involved in jumping sports such as volleyball, basketball and football. There is some evidence to suggest pathological tendon changes can begin in early adolescence if there excess load on the maturing collagen in the tendon.
Achilles tendon (back of heel)
Affects people across the lifespan, in particular long distance runners, sprinters, football and soccer players. Often there is pain and stiffness that is worse on waking and when running.
Gluteal tendon (side of hip)
Common in young females that are doing a lot of running or playing sport. Also older women, especially around menopause or after post a hip injury / surgery. Pain is often worse at night time, standing and walking. There is some research showing a reduction in oestrogen can pre-dispose to tendinopathy.
Hamstring tendon (back of hip)
Fast walkers, footballers, runners and people who do a lot of yoga are susceptible to hamstring tendinopathy. They often experience pain on sitting, walking and bending forwards.
What are the key risk factors for developing tendinopathy?
One of the biggest risk factors for a tendon injury is a past injury (2-19x greater risk of injury).
According to the research, people with tendon problems are not getting the rehabilitation and re-building of capacity they need.
Often patients self-discharge when their pain has gone away.
It is imperative for the treating clinician to educate the patient that rehabilitation is a two step process:
1. Reducing pain and then
2. Re-building capacity in the tissues to match the demands placed on them
Other systemic conditions that can increase the risk of developing tendon pain include:
Type 2 Diabetes ( 3 x risk)
High cholesterol
High blood pressure
Menopause
Obesity
Inflammatory arthropathies
Some other factors that put you at a higher risk of ongoing tendon pain:
unrealistic beliefs about likely healing time and optimal load management strategies
inaccurate beliefs pain e.g. avoiding movement due to fear or rupturing a tendon
too much passive treatment
reduced variability of movement / exercise
How is a diagnosis made?
Tendon issues are diagnosed with a combination of history and physical testing.
If you have a localised pain that gets worse with movement and you can recall a sudden change in loading, there is a good chance you have a tendon problem.
Do I need a scan?
Ultrasound scans can be useful to confirm the diagnosis and rule out certain other conditions.
(See below for more info on scans)
Recovery and Management :
1. Education ... (And Addressing Beliefs About Pain)
The long term goal is to create greater capacity in the tissues and this is your job, under the guidance of the physiotherapist looking after you.
Manual therapy and dry needling does have a role to play in the short term to decrease pain and normalise muscle tone.
Credit: Jill Cook
Pain and Pathology
You may have a scary sounding ultrasound report, with words such as 'severely degenerative'.
The bad news first. Your scans will most probably always look terrible.
Structurally over time, there will be no change, despite what you do in terms of treatment.
The good news:
Many high quality research studies have shown that there is no correlation between pain and structural changes on scans.
Your tendon will always be degenerated.
However, the thing we do have control over is the mechanical adaptation in the tissues around the tendon, as well as optimising biomechanics and sharing the load around the body.
The goal of treatment is to build the capacity in the tissues surrounding the tendon so that it meets the demand and creates a buffer zone of relaxation.
Some very important things to remember:
"Pathology is common in people without pain, so it cannot be the cause of pain.
Worse pathology does not mean it will be harder for you to get better.
Tendon pathology often does not change, even when the pain resolves" - Peter Malliaras
Recovery Time Line
It's important to understand the nature of recovery is often a case of 2 steps forward and 1 step back pattern.
It's normal for your pain levels to fluctuate.
If you can accept this, while continuing with your rehab, you will have a much greater chance of success.
Credit: Adam Meakins
2. Reduce the load temporarily while reducing pain and inflammation
Pain can be brought under control by managing load and using ice and NSAID's.
You may need to take a short break from any aggravating activities.
If you can't take anti-inflammatories you may need to look at your diet for areas to address inflammation.
How can isometrics help decrease pain?
Isometric refers to a static contraction of a muscle without any movement.
For example the diagram below shows an isometric contraction of the calf/achilles:
Benefits of isometric contractions in tendon healing (Malliaras et al 2013):
Isometrics can decrease pain without adding excess load to the tendon.
time under tension can be maximized to allow greater tendon strain, which is a likely stimulus for tendon adaptation
there is minimal soreness after doing isometrics, making them an ideal exercise 'during season'
loading can be performed in a range that is not painful and tendon compression can be minimized
The positive research around isometrics is in it's early stages and mainly focuses around the patella tendon.
3. Assess current load capacity and tolerance then begin re-loading the tendon.
Your Physiotherapist will take you through a comprehensive load capacity assessment and then develop a re-loading strategy.
This most important factor is that we progress the load over time to bring out positive adaptation and improved load tolerance.
You will most likely meet with your Physio once per week in the short term to closely monitor and progress the load at a suitable rate.
4. Clean up biomechanical issues and kinetic chain deficits
Biomechanical issues that may need addressing:
poor running technique
over-pronation
landing mechanics
postural issues
Kinetic chain deficits that may need addressing:
weak glutes
weak calves
weak quads
weak hamstrings, adductors
weak core
excessively tight muscles and joint restrictions
We will address these factors in the clinic. By optimising your movement efficiency, you will increase the likelihood of successfully returning to doing what you love and staying pain-free.
5. Progress the load and build capacity to greater than demand and gradually ease back into sport / exercise
This is where you get to really to push the boundaries of building capacity and gradually resume training and getting back to what you love.
It's important at this stage to think not only about training but also proper recovery to allow the tissues to optimally adapt.
You will want to optimise things like sleep, food / protein intake and foam rolling to keep your muscles tuned up.
This stage may weeks / months to fine tune and this is where we will monitor you loads to ensure a successful return.
In Summary - 5 Take Home Messages:
1. There Is Hope
Despite your ugly looking scan and long-term pain, there is good evidence to suggest you can make a good recovery and get back to doing what you enjoy.
2. It Takes Time
Tendons are resilient and adapt. But you need to give them time.
The time-frame on average to achieve this is a minimum of 12 weeks (but continual small improvements can still occur up to 5 years later).
3. Get Assessed By A Physiotherapist
There is a significant degree of complexity involved in a tendon problem and a Physiotherapist, after a comprehensive assessment will be able to guide you towards a positive outcome.
4. Only Exercise Can Increase Load Tolerance
"Your tissue capacity will only be as good as the load you put on it" - Professor Jill Cook
The end game is to build your resilience and capacity to create a 'buffer' zone of relaxation.
5. Think Quality Of Movement Before Quantity
Movement capacity develops step by step.
Small mindful movement of the muscle-tendon complex can improve efficiency and help ensure that your tendon issue becomes a thing of the past.
This is where Pilates can be very useful.
Pilates provides the perfect environment for sharpening the mind-muscle connection and also introduces elements of movement variability that help improve resilience.
Bonus Tips:
PRP injections are a waste of time
Steroid injections can have short term benefit but 12 months later can end up worse due to weakening of the tendon.
Fast walking can cause hamstring issues
For a tendon problem, generally it's best to avoid stretching
Hip bursitis is treated with same strategies as gluteal tendinopathy
Extracorporal Shockwave therapy is worth trying (more info about this click visit our friends at Adelaide Podiatry)
Thanks for reading this summary and if you have any questions or comments, please feel free to email dan@kinfolkwellness.com.au
If you have a tendon issue you would like to have assessed, I'd be honoured to help guide you.
You can make a booking using our easy online system here.