Hi, I’m Dan O'Grady, Physiotherapist, Running Coach, and Former PHT Sufferer
Are you an endurance runner who is tired of battling persistent buttock/hamstring pain that just won't quit?
As someone who has experienced the frustration of proximal hamstring tendinopathy (PHT) firsthand, I understand the challenges you're facing.
But I'm here to tell you that there is hope, and I'm ready to guide you every step of the way.
With over 20 years of experience working with runners and athletes, I've developed a proven approach to not only eliminate PHT but also enhance your running performance beyond what you thought possible.
As your dedicated coach and mentor, I'll provide personalized support and guidance to help you reclaim your love for running and enjoy life to the fullest once again.
This isn't just another cookie-cutter program—this is a supported self-management journey with me, Dan O'Grady, by your side.
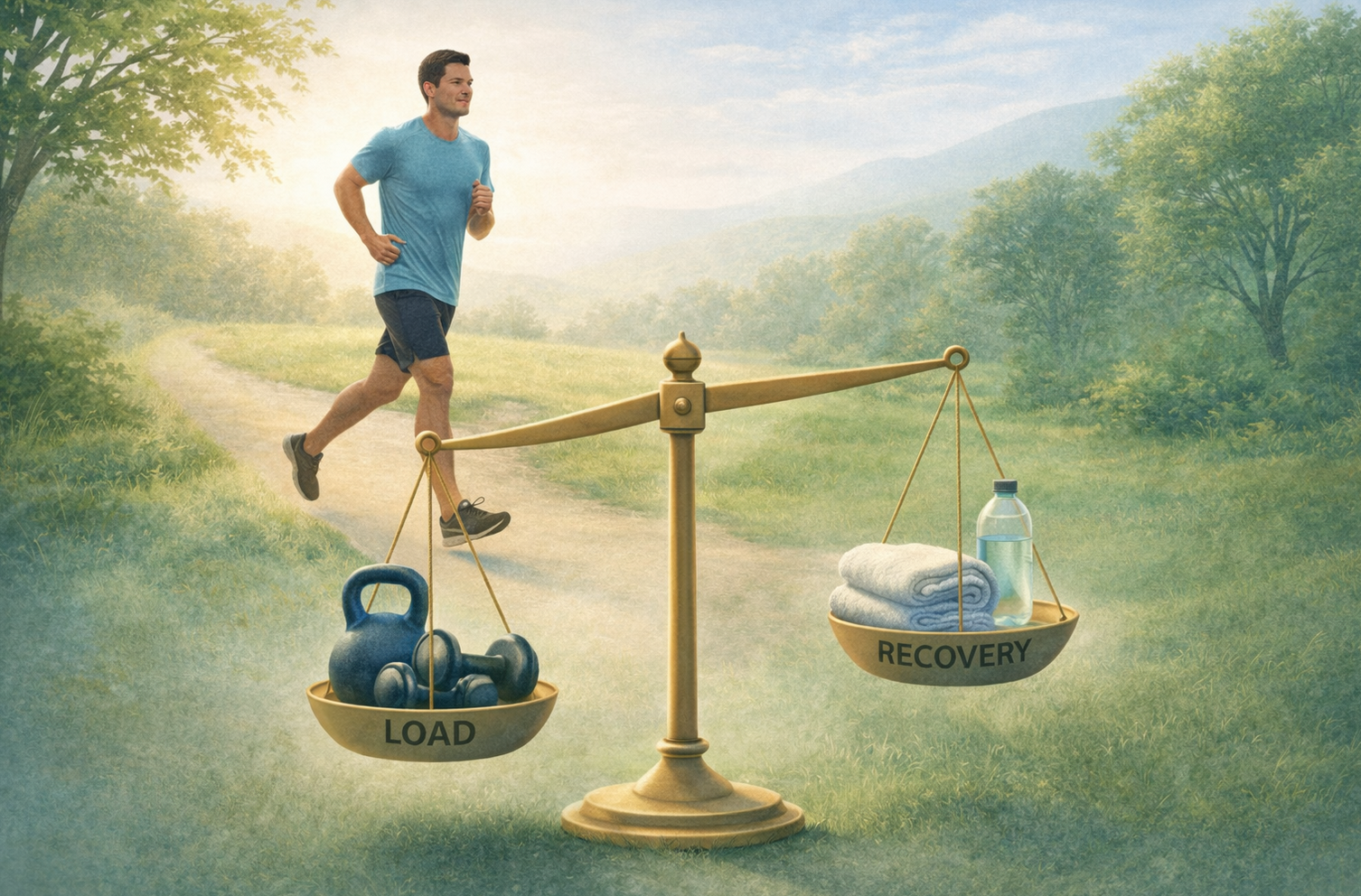
Using the framework of The Healthy Hamstring Protocol, we'll navigate through the ups and downs, teaching you what to avoid, how to improve your running technique, and how to efficiently recover from PHT.
And here's the best part:
I guarantee that you'll be back to running from day one, with a vision of growing to be stronger and more resilient than ever before…
So if you're ready to commit to your recovery and take your running to new heights, I'm excited to embark on this journey with you.
Spaces are limited….so don't miss out on the opportunity to transform your running experience.
Let's make it happen together—let's get you back to running and enjoying life, guaranteed
Next step, schedule a free 15 min phone call / zoom session with me at your convenience by following this link. Then we can decide if you’re the right fit for my unique and innovative program.
This program is available in person or any in the world through an app based online coaching portal.
You can also email dan@kinfolkwellness.com.au for any questions.