This week I did something rather foolish - I spiked my training load in a big way.
As you can see below on the graph, on the right of the screen was my run on Wednesday - a long 30km run.
That was a big increase from anything in the past few months.
My current training plan does involve building up to include more endurance, and I had planned on running somewhere from 20-25km this day.
But on a very cold winters day, with the sun shining and a nice coffee in my system, the running seemed effortless and I just wanted to keep running for the sheer joy and enjoyment of it - a soul run of sorts.
Yes I realize big increases in training load put you at risk of injury.
So I consciously made the decision to go for the longer distance and then see how the body responded.
The main goal for the 24-48 hours after a spike in load is to create an optimal environment for positive adaptation and growth to occur and to minimize the negative effects.
This is where active recovery can make a HUGE difference rather than just resting and feeling sore and sorry for yourself.
Over the years, I have experienced a few spikes in load - and now I think I am managing them somewhat better, so here are my top 5 tips to successfully manage a big spike in load:
Favor heat over cold
Previously I used to head straight for the cold water baths.
Whilst I think that can be useful for acutely painful spots, now I gain much more benefit from warm baths to help increase circulation to the legs. Throw in some epsom salts to help relax the muscles even more.
2. Increase protein and carbohydrate intake
At every opportunity I will add protein to meals and at snack times. I have a shake (30g protein) first thing in the morning and then eat good quality proteins through the rest of the day. Some other examples - hard boiled eggs, high protein yoghurt and protein bars. Mid afternoon I often will feel quite hangry so I add some extra carbohydrates into the mix.
3. Get on the foam roller
This can be hard to do because you know it’s going to be pretty ugly.
But if you can get some pressure onto the legs, it definitely helps with recovery.
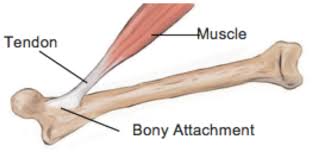
As muscles recover you want them to stay pliable.
If you don’t get in there with the roller or some massage, there is a greater chance for muscles to develop knots and trigger points, that can restrict range of motion and put pressure on joints - especially around the knee.
4. Sleep
Try and get a bit of extra sleep if you can by going to bed earlier or stay in bed a bit longer.
5. Light cardio
Some light walking/hiking and gentle core / pilates exercises help increase circulation and helps recovery.
After a big spike in load - you will definitely need to avoid high impact training for a few days or even up to a week.
Things to AVOID after a big spike in load
The things I would recommend you avoid:
heavy intense stretching
using non-steroidal anti-inflammatory
cold baths (although icing hot spots can be good)
lots of alcohol
Summary
Overall, I think spikes in load are a normal part of training.
Spikes in load can be very useful in fact as during the recovery - you can find out where your weak links are (the sorest spots) and perhaps add in some extra strength work to build resilience and anti-fragility.
Although they shouldn’t happen too often - I think if you can set up the optimal environment - you will come out feeling better than before.
You need to monitor your response to training for the next 1-2 weeks after a big spike as your body can still be a little vulnerable through the recovery period.
I hope that helps with your training and please let me know in the comments if you have any other tips.