Tendon pain, particularly chronic Achilles tendinopathy, is a challenging condition that can disrupt an active lifestyle especially for runners.
In recent years, researchers have delved into the metabolic underpinnings of tendon pain, shedding light on the role of lactate concentrations.
The Lactate Connection
Lactate, a compound associated with muscle fatigue and soreness, has emerged as a crucial factor in the study of painful chronic Achilles tendinopathy.
A study utilizing microdialysis techniques revealed higher concentrations of lactate in Achilles tendons afflicted by tendinopathy compared to healthy, pain-free tendons.
The significance of this finding lies in the revelation of anaerobic conditions within the painful tendon area.
Understanding the Results
The study's results are a piece of the intricate puzzle of tendon pain.
Let's break down what we can glean from this research:
Lactate Accumulation: The higher concentrations of lactate in painful tendons suggest that anaerobic conditions prevail in the affected area. This accumulation of lactate reflects a metabolic imbalance within the tendon, which may contribute to pain perception.
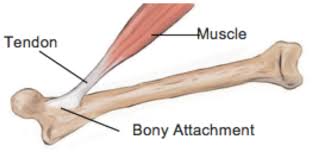
Tendon Structure: The study noted structural changes and widening of the tendon in cases of tendinosis. These observations are vital in understanding the pathological processes at play in chronic Achilles tendon.
A Holistic Approach to Tendon Pain Management
Understanding the metabolic basis of tendon pain is just the first step.
To effectively manage and alleviate this pain, we must take a holistic approach:
Training Load and Periodization: In the world of sports and physical activity, it's essential to adopt a balanced training load. The 80/20 principle, where 80% of training is in zone 2 (aerobic), can help minimize the risk of overuse injuries like tendinopathy.
Lactate Clearance: Optimal lactate clearance is key. Encourage activities that enhance lactate clearance, such as low-intensity exercise, adequate recovery periods, and proper hydration.
Therapeutic Modalities: Various therapeutic modalities can play a role in tendon pain management. These include massage, dry needling, and foam rolling, which can aid in reducing muscle tension and promoting blood flow to the affected area.
Liver and Kidney Health: Metabolic health is crucial. Liver and kidney health is vital for efficient metabolite clearance, including lactate. Ensure a balanced diet, stay hydrated, and minimize excessive alcohol consumption to maintain these organs' well-being.
Hydration: Proper hydration is essential to support overall metabolic processes, including lactate clearance. Staying adequately hydrated aids in reducing the risk of metabolic imbalances contributing to tendon pain.
Conclusion
The metabolic basis for tendon pain, as revealed in the study, offers valuable insights into the pathogenesis of chronic Achilles tendinopathy.
However, it's only one piece of the puzzle. To effectively manage tendon pain, we must adopt a holistic approach.
This approach includes optimizing training load, prioritizing lactate clearance, and utilizing therapeutic modalities to promote pain relief.
Furthermore, maintaining overall metabolic health through hydration and balanced nutrition is paramount.
As we continue to unravel the intricate nature of tendon pain, adopting a holistic approach can help individuals regain their active lifestyles and harmonize with their bodies' natural healing mechanisms.
Research link: High intratendinous lactate levels in painful chronic Achilles tendinosis. An investigation using microdialysis technique