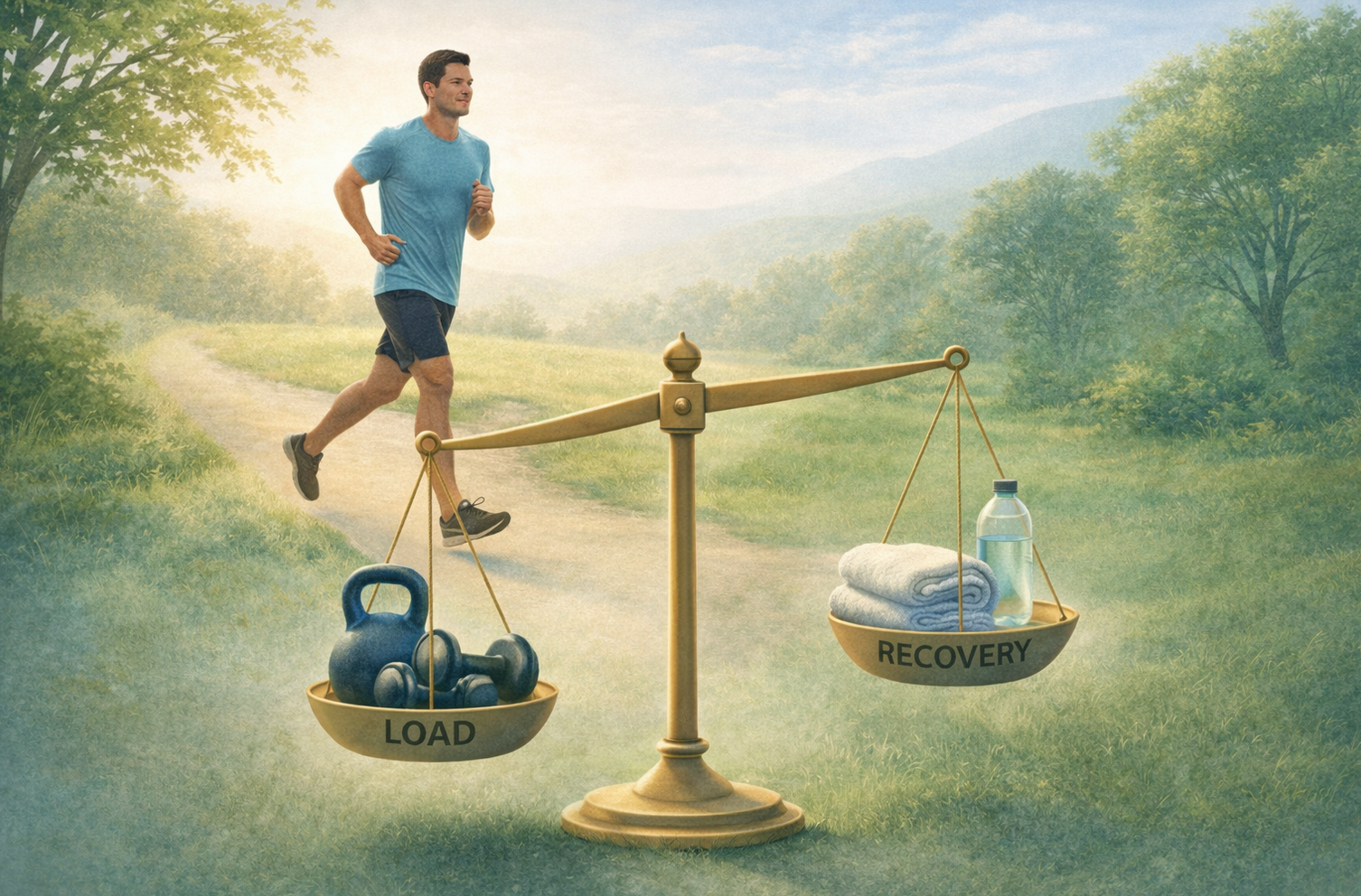
Scott Dye’s envelope of function is a way to visualize the safe loading zone for your knee.
Imagine your knee has an “envelope” or boundary that defines what combination of load (intensity of stress) and frequency (how often or how long) it can handle without getting irritated.
Inside this envelope, everything stays in homeostasis – a state of balance where tissues are happy and not signaling pain. For example, gentle activities like sitting, walking, or a short bike ride are usually within the envelope (low load, or low load over time) and don’t cause pain.
But if you do something outside your knee’s envelope – say, a very high load (like jumping from a height) or a moderate load done too frequently (like hours of basketball on an unconditioned knee) – you exceed what your knee can tolerate.
The knee tissues lose their comfortable equilibrium, and you may start to feel pain.
Crucially, pain in this context is a warning signal, not an announcement of catastrophic damage.
Dye hypothesized that “pain is the result when load applied to musculoskeletal tissues exceeds the ability to maintain homeostasis”.
In other words, when you go beyond what your joint can handle (outside the envelope), the tissue becomes stressed (out of balance) and your knee protests with pain.
If you ease up and let the knee return to its envelope of function, homeostasis can be restored and the pain will calm down.
Think of it like your knee’s way of saying, “Hey, that was too much for me – I need a break.”
Once you give it that break (reducing load, taking some rest), the knee often settles as balance is regained.
This perspective can be a huge relief.
It means your knee pain is understandable and manageable – it’s not random, and it doesn’t necessarily mean you’ve permanently injured something.
It’s more like an “overdraft alert” on a bank account: you spent a bit more (load) than your balance (capacity), and the bank (your body) is warning you to cut back.
Just as you’d get back on budget to avoid fees, with your knee you’d scale back to avoid pain.
The good news is that, just as budgets can improve, your knee’s envelope can expand with time and the right approach – but first, you have to stop overdrawing it.
What Should You Avoid? Finding Relief by Staying Within Your Envelope
One of the most empowering aspects of Dye’s approach is learning what NOT to do – identifying which activities are pushing your knee past its comfort zone.
Patients often find that when they stop the specific motions or exercises that aggravate the knee, the persistent pain diminishes. It’s not about becoming inactive; it’s about being smart and avoiding over-activity (or certain high-stress moves) until your knee can handle them.
So, what activities tend to lie outside the envelope for someone with anterior knee pain? Here are a few common culprits to be cautious about:
Deep squats or lunges (especially with heavy weight or poor form): These can put very high pressure on the kneecap and cartilage. Doing too many, too deep, or too fast is a classic way to overload the patellofemoral joint. Dye notes that “excessive squats and lunges” prescribed by well-meaning but uninformed trainers or therapists can easily worsen knee pain. If your knee is hurting, it’s wise to avoid deep knee bends for now – or only do them in a pain-free range of motion.
Running stairs or hills, or high-impact jumping: The impact forces when you run downhill or jump and land can spike above what an irritable knee can tolerate. These high-load, repetitive impacts can quickly exceed your knee’s envelope if you’re already sensitized. It might be better to stick to flat surfaces or low-impact cardio (like cycling or swimming) while your knee recovers its balance.
Prolonged kneeling or deep knee bending postures: Many people with patellofemoral pain feel increased ache when the knee is bent deeply for a long time (for example, crouching, or sitting in a tight seat at the movies). This sustained pressure can aggravate the joint. Take breaks to stretch your leg out, or avoid those positions for long durations.
Too much, too soon – even of “good” activities: Even beneficial exercise can overshoot the mark if overdone. A classic example is a well-intentioned physical therapy regimen that is too aggressive. If exercises given for rehab consistently cause sharp pain or swelling after, they may be beyond your current envelope. As Dye’s common-sense approach advises, treatment should never encourage pushing through pain or making symptoms worse.
By identifying your personal triggers, you gain clarity on what movements load your kneecap or joint the most.
Many patients feel a sense of relief that they’re not dealing with a mysterious problem – it becomes clear that “Okay, 50 lunges were too many” or “Jogging 5 days a week is flaring my knee”.
This relief comes from understanding that by simply avoiding or modifying those specific stressors, you can significantly reduce your pain. For instance, one young athlete with knee pain might realize that cutting basketball down to 30 minutes instead of 2 hours, and swapping some practices for biking, allows the knee to stay pain-free.
Another office worker might find that adding breaks during long sitting or using a standing desk part-time keeps their knee happier. These adjustments keep you within your knee’s envelope of function, preventing that “loss of homeostasis” that triggers pain.
Importantly, staying within your envelope is not about never moving your knee or being fearful of activity.
In fact, complete rest isn’t the goal – that can lead to deconditioning, which actually shrinks your envelope over time.
Instead, the aim is to keep doing pain-free activities (to maintain fitness and confidence) while temporarily avoiding the pain-triggering ones.
It’s a bit like avoiding potholes on a road: drive around the pothole (find an alternate activity) rather than keep hitting it and damaging your tire.
Meanwhile, you can work on gradually repairing the road (rehabbing your knee) so that pothole isn’t such a problem in the future.
Challenging the Old “Damage = Pain” Myth (and Avoiding Unnecessary Treatments)
Dye’s approach also challenges some outdated ways of thinking about knee pain.
Traditionally, if you had anterior knee pain, doctors would look for something structurally “wrong” – often blaming chondromalacia patellae (a softening or wear of the cartilage under the kneecap) or saying your kneecap was misaligned.
The treatment might have been surgery to “fix” the cartilage or realign the kneecap, or rigorous physical therapy to strengthen and force changes.
Unfortunately, many patients went through these invasive or intensive interventions only to find their pain persisted or even worsened.
Scott Dye observed that the old purely biomedical model – focusing only on fixing cartilage or alignment seen on an MRI – was incomplete.
Pain isn’t always proportional to visible structural changes.
In fact, Dye famously proved this in an extraordinary experiment on himself: he underwent an arthroscopic examination of his own knee without anesthesia (so he could feel what hurt and what didn’t).
The scope revealed significant cartilage wear (Grade 3 chondromalacia) in his knee, yet when the surgeon probed that supposedly “damaged” cartilage, he felt no pain at all!
Why?
Because cartilage itself has no nerve supply – it’s aneural – so it cannot directly cause pain.
This means that a rough-looking kneecap on an MRI isn’t a guaranteed pain generator.
Oftentimes, it’s the overloading of the joint – and the stress on the bone or synovial tissue around the cartilage – that actually produces pain, not the cartilage wear itself.
Dye’s tissue-homeostasis perspective explains why many surgeries for knee pain have disappointing results.
If a patient’s pain was due to exceeding their envelope (functional overload), then simply shaving off cartilage or “fixing” a patella alignment doesn’t address the root cause – it might even introduce more trauma.
As Dye pointed out, “many of the worst knee pain cases are iatrogenic” – meaning caused by medical interventions – often stemming from surgeries aimed at correcting chondromalacia or malalignment that weren’t actually the true pain.
Likewise, overly aggressive rehab exercise protocols, applied under the false belief that a patient just needs to “strengthen through the pain,” have left some people worse off than before.
It’s tragic but true: well-intentioned treatments can backfire if they’re based on a misunderstanding of the pain’s cause.
The envelope of function model steers us back to a safer, gentler approach.
Rather than immediately resort to surgical scopes, cartilage smoothing, or forcing heavy exercises, it advocates activity modification and patience first.
This approach is often very effective: Many patients improve with simple measures like unloading the joint (resting from painful activities), doing pain-free range exercises, and gradually reintroducing load – all while not doing anything that consistently aggravates the knee.
As Dye’s team put it, this is a “common sense” approach that acknowledges healing is a biological process that takes time, especially in a high-stress area like the knee.
It also aligns with the medical principle “first, do no harm.”
By avoiding high-risk interventions and respecting the knee’s limits, you minimize the chance of making things worse. In short, don’t poke the bear – let it calm down.
For you as a patient, this should feel empowering. It means you’re not automatically doomed to surgery or stuck with bad cartilage.
With knowledge and prudent care, you can often get better by working with your body’s natural healing capacity.
Of course, every case is unique – and sometimes surgical or specialized interventions are truly needed – but even then, understanding the envelope concept will help in rehab and preventing re-injury.
Pain as a Homeostatic Emotion: Your Body’s Built-In Alarm System
You might be wondering, “Okay, I get that doing too much causes pain. But what actually is pain in this context? Why does it hurt, and what does that mean?”
This is where we bring in neuroscientist A.D. “Bud” Craig’s idea of pain as a “homeostatic emotion.”
It sounds fancy, but the core idea is actually pretty intuitive – and it complements Dye’s envelope model perfectly.
Craig’s research suggests that pain is not just a physical sensation like touch, but also an emotion or motivation that our brain creates to help protect us.
In an influential paper, he explained that “the human feeling of pain is both a distinct sensation and a motivation – that is, a specific emotion that reflects a homeostatic behavioral drive, similar to temperature, itch, hunger and thirst”.
In simpler terms, pain is your body’s way of urging you to take care of something, just like hunger is your body’s way of telling you to eat to keep your system in balance.
Think of some examples of “homeostatic emotions” in everyday life:
Hunger: an uncomfortable feeling that motivates you to eat and restore energy balance.
Thirst: a powerful urge that makes you drink fluids to rehydrate.
Feeling cold: prompts you to put on a sweater or seek warmth to keep your temperature stable.
Now, pain can be seen in a similar light.
If you’ve done a bit too much with your knee (tipping it out of its happy equilibrium), pain is the resulting feeling that motivates you to change something – to rest, to move differently, or to avoid that stress – in order to protect your tissues and let them recover.
It’s essentially an alarm or warning signal.
Not a false alarm, and not a punishment, but a helpful (if unpleasant) indicator that something needs adjusting to maintain the health of the system.
This view of pain is actually very reassuring.
It means your pain has a purpose and meaning: it’s trying to keep you safe and balanced.
When your knee “hurts for no obvious reason,” it might simply be that the tissues were strained (even microscopically) beyond their comfort zone, and your brain generated pain to say “slow down.”
It’s akin to the way your muscles burn during a workout as a signal to not push too far – except knee pain might show up hours after the fact, when your body processes the inflammation or stress.
Bringing it back to the envelope of function: Bud Craig’s concept gives the neurological explanation for what Scott Dye described mechanically.
Dye said: “go beyond tissue homeostasis, and you’ll get pain”.
Craig is saying: yes, and that pain is your brain’s tool to drive behavior (like resting) to restore homeostasis.
They’re two sides of the same coin.
Your knee pain is meaningful – it’s your body’s built-in safety feature, much like a thermostat triggers the AC if things get too hot.
When you respect it, you can use it to guide your activity levels and gradually improve.
A More Empowering Approach: Listening to Pain Without Fear
By combining Dye’s and Craig’s ideas, we get a powerful, patient-friendly model for managing pain – one that contrasts with both the old biomedical approach and some newer “pain is in the brain” narratives.
Here’s how this combined model can help you, and why it might make you feel more hopeful:
Pain is Real, But Not a Mystery: Unlike a pure biomedical view, we’re not solely chasing structural “damage” on an MRI; and unlike a pure pain neuroscience view, we’re not saying pain is just a misfiring alarm divorced from the body.
Instead, we acknowledge that pain often has a real mechanical/traditional trigger (load on tissues) and a real biological purpose (to warn and protect). This means you don’t have to feel crazy if you hurt but doctors say “nothing is wrong” – something was wrong: your knee did too much! It just might not show up as a tear or break. Conversely, if your scans do show wear-and-tear, you don’t have to panic – those changes might not be causing the pain at all if you stay in homeostasis.
You Have Control Through Behavior: This model puts a lot of the power in your hands. If pain is largely about whether you’re within your knee’s envelope, then by modifying your activities (how much, how intense, how often) you can directly control a lot of your pain. This is far more empowering than feeling like you need a surgeon to “fix” you, or that you’re at the mercy of a pain that has “a life of its own” in your nerves. Simple adjustments – like swapping high-impact exercises for low-impact ones, pacing yourself, and slowly building tolerance – can pay off hugely. As one research group succinctly stated, patients with anterior knee pain “frequently respond well to load restriction that protects their knee and reduces pain during rehabilitation”.
In plainer words, backing off the stressful activities lets the knee calm down so it can heal – a straightforward strategy that often works.
“It’s Not All in My Head”: Some modern pain education can sometimes leave patients feeling like they’re being told the pain is just a false alarm or a psychological trick. While it’s true that the brain plays a big role, pain neuroscience education (PNE) done poorly can make people anxious or feel dismissed – like being told to ignore pain because “pain does not equal harm.” In reality, pain can be a very useful signal of something that needs addressing. One patient advocate described how the “just ignore it” approach went wrong for her: “For years I... calmly [did] stuff I really should not have been doing. My body was sending the right signal, not a false alarm.” She was acting out of a rational response to pain (her body asking her to stop), not irrational fear. The envelope/homeostasis model validates your pain – it says, “We hear you; your pain is telling us something and we’ll use that information.” Patients often feel relief when their pain is taken seriously as a protective response, rather than brushed off.
Reducing Anxiety by Understanding Pain: When you know that pain is not necessarily equal to tissue destruction, but rather a sign of tissue imbalance, you can stop catastrophizing every twinge. Instead of, “Oh no, my knee hurts going down stairs – maybe I’m tearing it more!” you can reframe it as, “Hmm, that’s outside my envelope right now, I should avoid too many stairs for a bit and do gentler exercise.” This understanding often reduces the fear and anxiety around pain. You realize you’re not in a downward spiral of damage – you’re in a manageable situation of sensitivity. Much like you wouldn’t panic that you have a permanent illness when you feel thirsty (you’d just drink water), you don’t need to panic that knee pain means you’re permanently broken – you may just need to adjust and let your knee’s balance restore. As a result, many people feel more confident and in control of their condition.
Moving Forward: Balancing Rest and Activity to Expand Your Envelope
With this knowledge, the path forward is all about balance and gradual progress:
In the short term, avoid the big aggravators that we identified – give your knee a chance to settle. This might mean taking a break from running or intense workouts and doing more gentle activities that keep you moving without pain (like walking, cycling, or swimming at a comfortable pace).
At the same time, don’t stop all activity. Total rest can make joints stiff and muscles weak. Instead, keep doing what you comfortably can. This maintains circulation, muscle tone, and your mood. As one blog put it, doing only tiny low-load activities and nothing else can cause deconditioning, shrinking your envelope further. So we want to find that sweet spot of “just right” activity – not too much, not too little.
Gradually reintroduce or increase load as tolerated. After a period of protection, your knee’s envelope can start to widen again. Maybe you can try a short hike or a few light squats and see how you feel the next day. The key is to increase in small steps and pay close attention to your knee’s feedback. If you stay pain-free, or only have mild soreness that resolves quickly, you’re likely still within a safe zone. If you get sharp pain or a big flare-up, you know you’ve likely crossed the line – pull back and give it more time. This stepwise approach is like gently expanding your knee’s comfort zone. Over weeks and months, those little gains add up – perhaps today you can’t squat without pain, but in a month of gradual strengthening and avoiding overload, you might be able to do a half-squat pain-free, and eventually full squats.
Educate your supporters (family, coaches, therapists). Sometimes well-meaning people might push you to do things that hurt (“No pain, no gain!”) or express skepticism (“The MRI showed nothing, so why does it hurt?”). Sharing what you’ve learned – that your pain is real and tied to function, not imaginary – can help them understand why you’re pacing yourself. You could mention that a leading knee surgeon proposed this model where pain is about going beyond what the knee can bear, and you’re following a sensible plan to stay within safe limits and build back up. Having others on board will make it easier for you to stick to the plan without pressure or doubt.
Above all, be patient and kind to yourself. Anterior knee pain, especially if it’s been around for a while, can take time to fully resolve. There may be ups and downs. But armed with the envelope of function concept and the knowledge that pain is your guide (not your enemy), you can approach your rehab intelligently. You’re not simply at the mercy of pain – you are working with your body’s signals to find a sustainable path forward.
Conclusion: Embrace the Balance and Take Charge of Your Knee Health
Scott Dye’s envelope of function and the idea of pain as a homeostatic emotion together paint a hopeful picture: your knee pain is not a random curse or an irreversible damage – it’s a sign of imbalance that can be corrected.
By respecting your knee’s current limits and avoiding the traps of overloading (or over-treating), you give it the best environment to heal. And by understanding pain’s true role, you replace fear with a sense of purpose – pain becomes a useful feedback, like a compass pointing you toward the right level of activity.
This approach offers a middle path between “babying” the knee and “boot-camp” style rehab.
It’s about smartly calibrating your activities.
You’ll find that sweet zone where your knee is comfortable, and then gently push that envelope outward over time. Many patients find that, as they do this, their confidence returns: “Hey, I walked 2 miles today and still feel okay – a few weeks ago even 1 mile hurt.”
Those little victories build up.
Remember, healing is rarely overnight.
But each day you follow these principles, you are likely improving your knee’s capacity bit by bit.
On the tough days, remind yourself that pain is not a setback so much as information – it’s telling you that something was too much. Adjust, stay positive, and know that you’re working with your body’s natural system.
In summary, Scott Dye’s unique approach reframes knee pain from a terrifying sign of damage to a manageable problem of comfort zones and balance.
And the concept of pain as a homeostatic emotion reassures you that your pain is meaningful and not just “in your head.”
Together, these ideas give you a clearer roadmap.
Instead of feeling anxious or confused, you can feel empowered to make the right choices for your knee.
With time, knowledge, and patience, you can help your knee find its happy equilibrium again – and get back to the activities you love, at a pace that’s right for you.
References:
Dye SF. The knee as a biologic transmission with an envelope of function: a theory. Clin Orthop Relat Res. 1996;325:10-18. (Introduction of the envelope of function concept)pubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov
Dye SF, et al. Patellofemoral pain: an enigma explained by homeostasis and common sense. Orthopedics. 2013. (Article discussing tissue homeostasis and envelope of function in anterior knee pain)community.the-hospitalist.orgcommunity.the-hospitalist.org
Dye SF. Lessons from an anterior knee pain pioneer. Interview/Article, MDedge (The Hospitalist). 2017. (Insights from Scott Dye, including the envelope of function and critique of outdated approaches)community.the-hospitalist.orgcommunity.the-hospitalist.org
Craig AD. A new view of pain as a homeostatic emotion. Trends Neurosci. 2003;26(6):303-307. (Research article describing pain as an emotion that reflects a homeostatic drive)pubmed.ncbi.nlm.nih.gov
Physiotutors Blog. The Envelope of Function – Overuse Injuries Explained. 2023. (Patient-friendly explanation of envelope of function with examples)physiotutors.comphysiotutors.com
Stoops K, quoted in Ingraham P. The dark side of Explain Pain – gaslighting pain patients with PNE. PainScience.com blog, 2023. (Patient perspective on the misuse of pain neuroscience education)painscience.com
Esculier JF, et al. How to manage patellofemoral pain – Understanding loading mechanisms. JOSPT Blog, 2020. (Recommends load management and activity modification in treating kneecap pain)journals.sagepub.com