The past weekend I attended Peter Malliaras's course, 'Mastering Lower Limb Tendinopathies'.
Peter is an Associate Professor at Monash University and has spent many years researching and working with people with tendon problems.
In recent years there has been a lot of significant new research in the world of tendon rehab.
If you've ever had an issue with an ongoing tendon problem, you can understand how frustrating the long term pain and dysfunction can be.
There is much conflicting advice and out dated treatment approaches that can contribute to the poor outcomes many people face with tendon injuries.
Thankfully, Peter has put all of the latest based evidence into a comprehensible format and in this blog post I'd like to share just a little summary.
This blog would be particularly helpful if you suffer from ongoing pain in the:
Achilles tendon
Hamstring
Patella tendon
Hip pain/bursitis
Plantar fascia
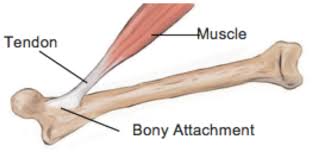
What is a tendon?
Tendons connect the muscle to bone. They are made up primarily of collagen fibres.
In the lower limb, role of tendon is to absorb and release energy
Tendons are like springs that absorb stretching forces and then release energy when we move.
What causes tendon problems?
Tendons are very sensitive to changes in load.
Essentially, tendons become injured when we over-load them too soon, or when demand exceeds capacity.
This can be from:
too much volume
too much intensity
change in footwear or surface
For example a runner may start to include sprinting or hill work too soon or increase mileage suddenly leading up to a big race.
High training load is not a risk for injuries, it's how you get there that is the important factor (i.e. avoiding acute spikes in training loads).
Tendons become damaged when demand exceeds their capacity
What is the difference between Tendinitis and Tendinopathy?
Tendinitis refers to the inflammation in the early stages of an injury.
This is opposed to tendinopathy that refers to the process of degeneration that tendon goes through in response to chronic overload.
Recent research suggests a lot of what we previously thought of as tendon inflammation was actually related to tendinopathy.
Who is likely to suffer from a tendon problem?
Patella tendon (front of knee)
Usually occurs in younger people involved in jumping sports such as volleyball, basketball and football. There is some evidence to suggest pathological tendon changes can begin in early adolescence if there excess load on the maturing collagen in the tendon.
Achilles tendon (back of heel)
Affects people across the lifespan, in particular long distance runners, sprinters, football and soccer players. Often there is pain and stiffness that is worse on waking and when running.
Gluteal tendon (side of hip)
Common in young females that are doing a lot of running or playing sport. Also older women, especially around menopause or after post a hip injury / surgery. Pain is often worse at night time, standing and walking. There is some research showing a reduction in oestrogen can pre-dispose to tendinopathy.
Hamstring tendon (back of hip)
Fast walkers, footballers, runners and people who do a lot of yoga are susceptible to hamstring tendinopathy. They often experience pain on sitting, walking and bending forwards.
What are the key risk factors for developing tendinopathy?
One of the biggest risk factors for a tendon injury is a past injury (2-19x greater risk of injury).
According to the research, people with tendon problems are not getting the rehabilitation and re-building of capacity they need.
Often patients self-discharge when their pain has gone away.
It is imperative for the treating clinician to educate the patient that rehabilitation is a two step process:
1. Reducing pain and then
2. Re-building capacity in the tissues to match the demands placed on them
Other systemic conditions that can increase the risk of developing tendon pain include:
Type 2 Diabetes ( 3 x risk)
High cholesterol
High blood pressure
Menopause
Obesity
Inflammatory arthropathies
Some other factors that put you at a higher risk of ongoing tendon pain:
unrealistic beliefs about likely healing time and optimal load management strategies
inaccurate beliefs pain e.g. avoiding movement due to fear or rupturing a tendon
too much passive treatment
reduced variability of movement / exercise
How is a diagnosis made?
Tendon issues are diagnosed with a combination of history and physical testing.
If you have a localised pain that gets worse with movement and you can recall a sudden change in loading, there is a good chance you have a tendon problem.
Do I need a scan?
Ultrasound scans can be useful to confirm the diagnosis and rule out certain other conditions.
(See below for more info on scans)
Recovery and Management :
1. Education ... (And Addressing Beliefs About Pain)
The long term goal is to create greater capacity in the tissues and this is your job, under the guidance of the physiotherapist looking after you.
Manual therapy and dry needling does have a role to play in the short term to decrease pain and normalise muscle tone.
Credit: Jill Cook
Pain and Pathology
You may have a scary sounding ultrasound report, with words such as 'severely degenerative'.
The bad news first. Your scans will most probably always look terrible.
Structurally over time, there will be no change, despite what you do in terms of treatment.
The good news:
Many high quality research studies have shown that there is no correlation between pain and structural changes on scans.
Your tendon will always be degenerated.
However, the thing we do have control over is the mechanical adaptation in the tissues around the tendon, as well as optimising biomechanics and sharing the load around the body.
The goal of treatment is to build the capacity in the tissues surrounding the tendon so that it meets the demand and creates a buffer zone of relaxation.
Some very important things to remember:
"Pathology is common in people without pain, so it cannot be the cause of pain.
Worse pathology does not mean it will be harder for you to get better.
Tendon pathology often does not change, even when the pain resolves" - Peter Malliaras
Recovery Time Line
It's important to understand the nature of recovery is often a case of 2 steps forward and 1 step back pattern.
It's normal for your pain levels to fluctuate.
If you can accept this, while continuing with your rehab, you will have a much greater chance of success.
Credit: Adam Meakins
2. Reduce the load temporarily while reducing pain and inflammation
Pain can be brought under control by managing load and using ice and NSAID's.
You may need to take a short break from any aggravating activities.
If you can't take anti-inflammatories you may need to look at your diet for areas to address inflammation.
How can isometrics help decrease pain?
Isometric refers to a static contraction of a muscle without any movement.
For example the diagram below shows an isometric contraction of the calf/achilles:
Benefits of isometric contractions in tendon healing (Malliaras et al 2013):
Isometrics can decrease pain without adding excess load to the tendon.
time under tension can be maximized to allow greater tendon strain, which is a likely stimulus for tendon adaptation
there is minimal soreness after doing isometrics, making them an ideal exercise 'during season'
loading can be performed in a range that is not painful and tendon compression can be minimized
The positive research around isometrics is in it's early stages and mainly focuses around the patella tendon.
3. Assess current load capacity and tolerance then begin re-loading the tendon.
Your Physiotherapist will take you through a comprehensive load capacity assessment and then develop a re-loading strategy.
This most important factor is that we progress the load over time to bring out positive adaptation and improved load tolerance.
You will most likely meet with your Physio once per week in the short term to closely monitor and progress the load at a suitable rate.
4. Clean up biomechanical issues and kinetic chain deficits
Biomechanical issues that may need addressing:
poor running technique
over-pronation
landing mechanics
postural issues
Kinetic chain deficits that may need addressing:
weak glutes
weak calves
weak quads
weak hamstrings, adductors
weak core
excessively tight muscles and joint restrictions
We will address these factors in the clinic. By optimising your movement efficiency, you will increase the likelihood of successfully returning to doing what you love and staying pain-free.
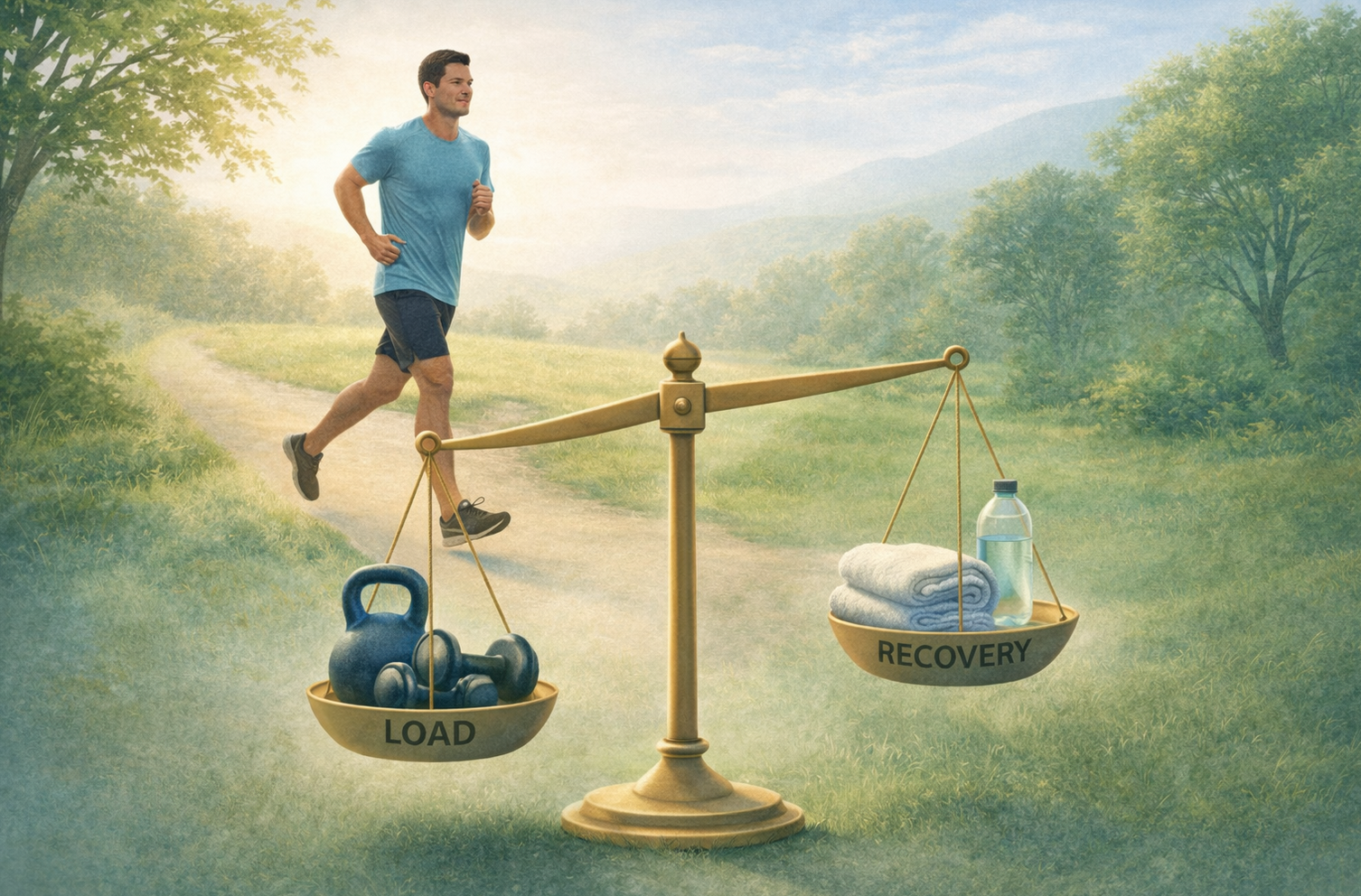
5. Progress the load and build capacity to greater than demand and gradually ease back into sport / exercise
This is where you get to really to push the boundaries of building capacity and gradually resume training and getting back to what you love.
It's important at this stage to think not only about training but also proper recovery to allow the tissues to optimally adapt.
You will want to optimise things like sleep, food / protein intake and foam rolling to keep your muscles tuned up.
This stage may weeks / months to fine tune and this is where we will monitor you loads to ensure a successful return.
In Summary - 5 Take Home Messages:
1. There Is Hope
Despite your ugly looking scan and long-term pain, there is good evidence to suggest you can make a good recovery and get back to doing what you enjoy.
2. It Takes Time
Tendons are resilient and adapt. But you need to give them time.
The time-frame on average to achieve this is a minimum of 12 weeks (but continual small improvements can still occur up to 5 years later).
3. Get Assessed By A Physiotherapist
There is a significant degree of complexity involved in a tendon problem and a Physiotherapist, after a comprehensive assessment will be able to guide you towards a positive outcome.
4. Only Exercise Can Increase Load Tolerance
"Your tissue capacity will only be as good as the load you put on it" - Professor Jill Cook
The end game is to build your resilience and capacity to create a 'buffer' zone of relaxation.
5. Think Quality Of Movement Before Quantity
Movement capacity develops step by step.
Small mindful movement of the muscle-tendon complex can improve efficiency and help ensure that your tendon issue becomes a thing of the past.
This is where Pilates can be very useful.
Pilates provides the perfect environment for sharpening the mind-muscle connection and also introduces elements of movement variability that help improve resilience.
Bonus Tips:
PRP injections are a waste of time
Steroid injections can have short term benefit but 12 months later can end up worse due to weakening of the tendon.
Fast walking can cause hamstring issues
For a tendon problem, generally it's best to avoid stretching
Hip bursitis is treated with same strategies as gluteal tendinopathy
Extracorporal Shockwave therapy is worth trying (more info about this click visit our friends at Adelaide Podiatry)
Thanks for reading this summary and if you have any questions or comments, please feel free to email dan@kinfolkwellness.com.au
If you have a tendon issue you would like to have assessed, I'd be honoured to help guide you.
You can make a booking using our easy online system here.