A new study has shown there is likely to be a 276 per cent rise in knee replacement procedures from 2013 to 2030 (based on data from Australia's joint replacement registry).
Pretty staggering ! 😱
The biggest risk factor for knee arthritis leading to a total knee replacement is being overweight, which overtime stresses the knee joints (70% of Aussies are overweight).
This article talks about your options, especially if you want to avoid surgery.
Main points 💥
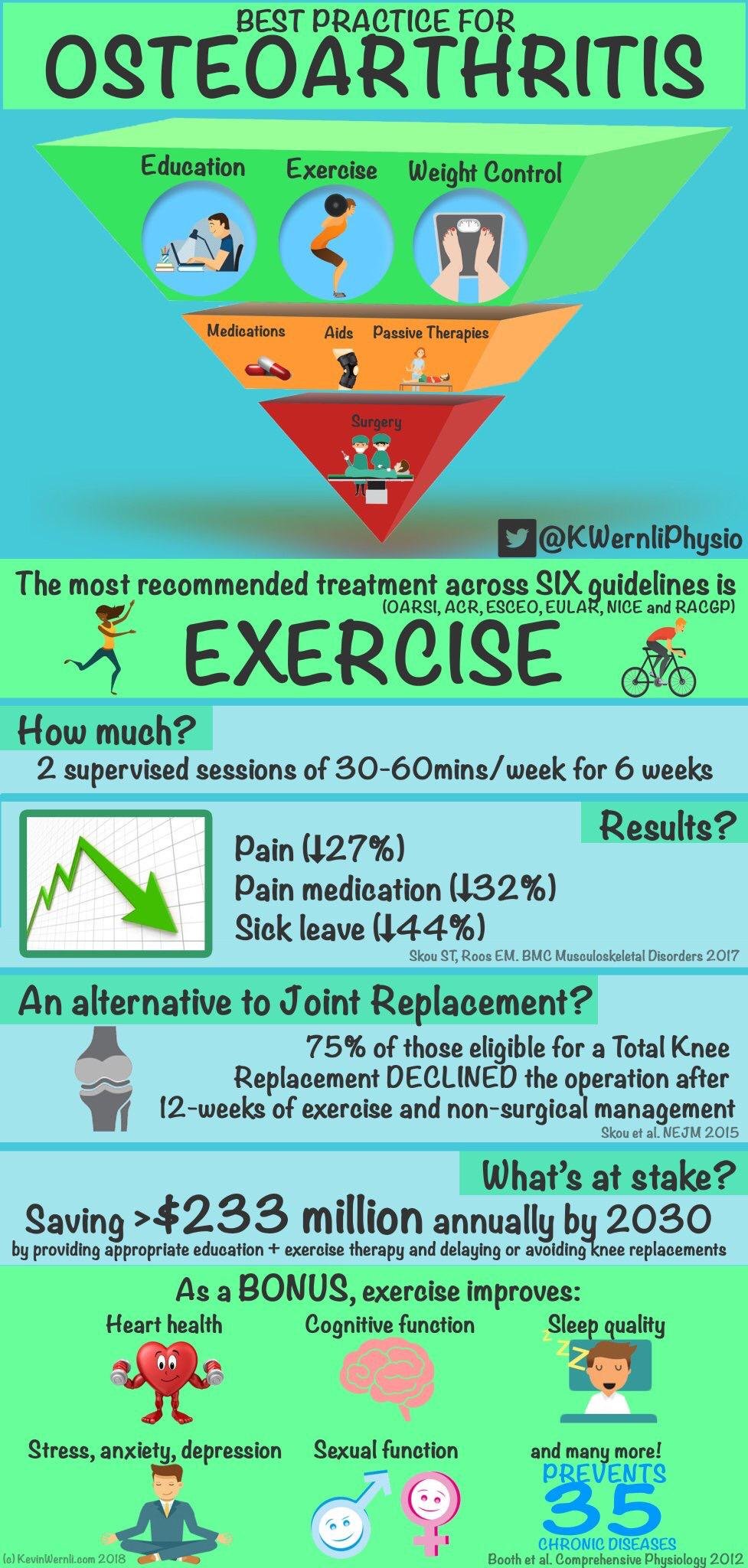
✅ Gradually increase your activity levels and incorporate targeted strengthening exercises to build the muscles around the knees.
✅ This can make them stronger, help to maintain appropriate co-ordination and reduce pain.
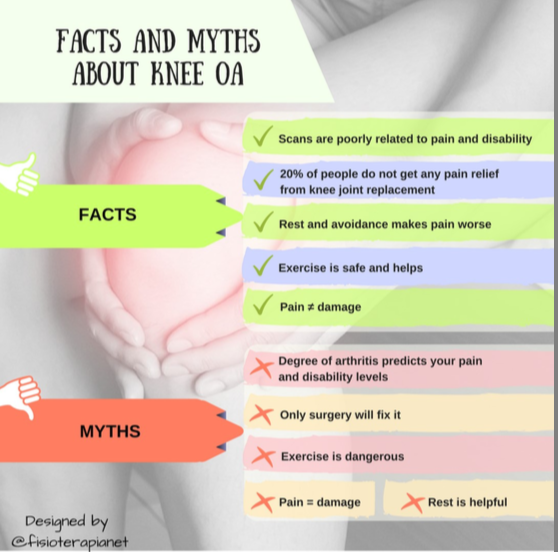
✅ Don't be fearful of exercise and movement, even if you do feel some pain. Pain doesn't equal damage.
✅ Running 💯% does not cause knee arthritis. On the contrary, runners have less chance of developing arthritis because they generally not overweight.
✅ Consult with your GP and Physiotherapist who can develop a customised plan to get you moving well again.
✅ Individual movement assessment can help you identify your weak links and help get you on the fast track.
✅ For more info about how Physio can help with your knee pain and get you moving well again 👇