Can You Run with Knee OA?
Here's What You Need to Know!
So you’ve just been diagnosed with knee osteoarthritis (OA)…
There may be many questions running through your head
What exactly is knee osteoarthritis (OA), and how did I get it?
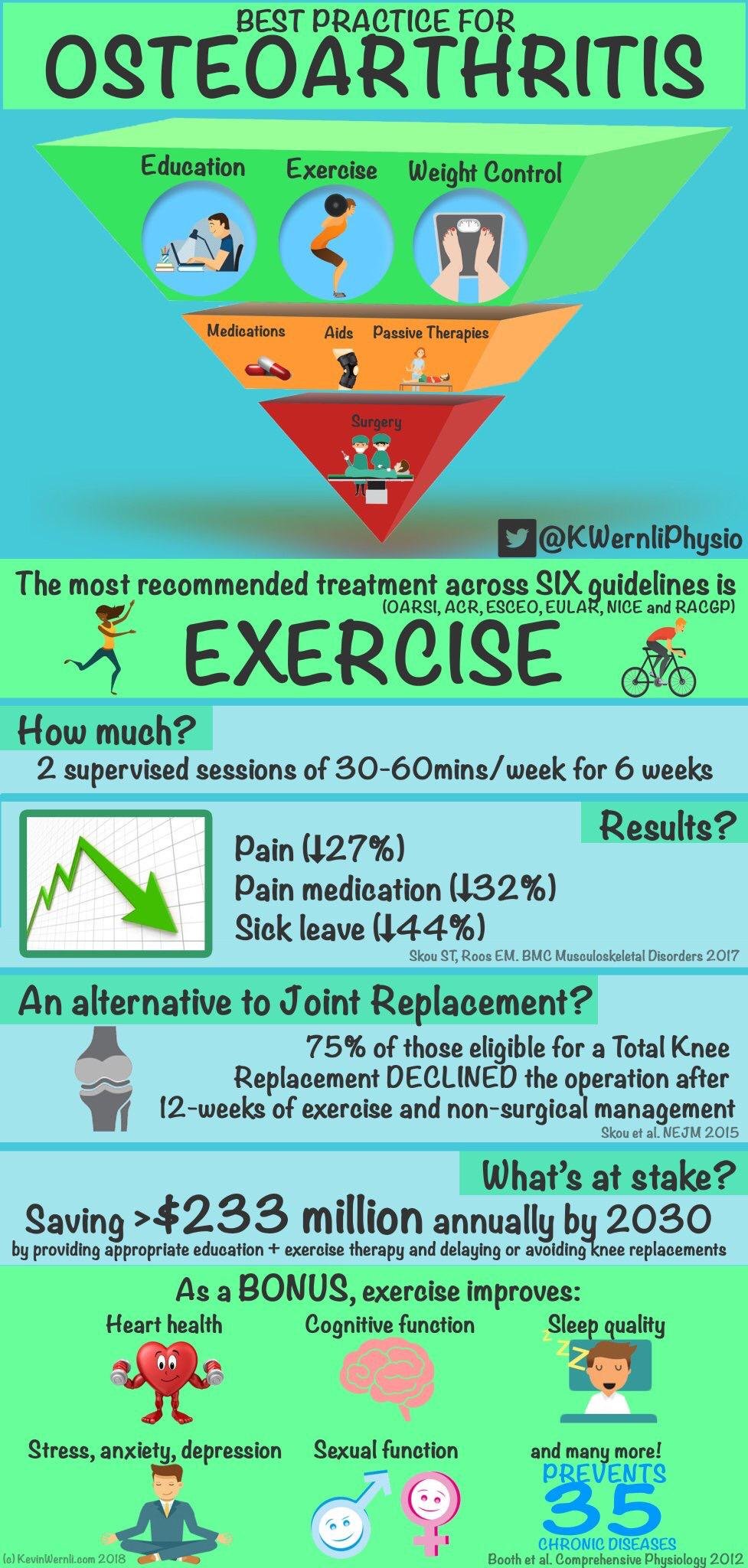
What are the best treatment options for managing knee OA?
Will I need surgery at some point, or are there other alternatives?
Can I use knee OA as an excuse to skip leg day at the gym forever?
Can I blame knee OA for my newfound ability to predict the weather with my knees?
But if you’re like me, your most important concern will be:
“Can I still lace up my running shoes and hit the pavement?”
Well, you're not alone!
Many folks in your shoes (pun intended) are curious about the same thing.
Let's dive in and explore whether running with knee OA is a good idea, and how it might even help ease your knee pain.
Understanding Knee Osteoarthritis (OA):
First off, let's talk about knee OA.
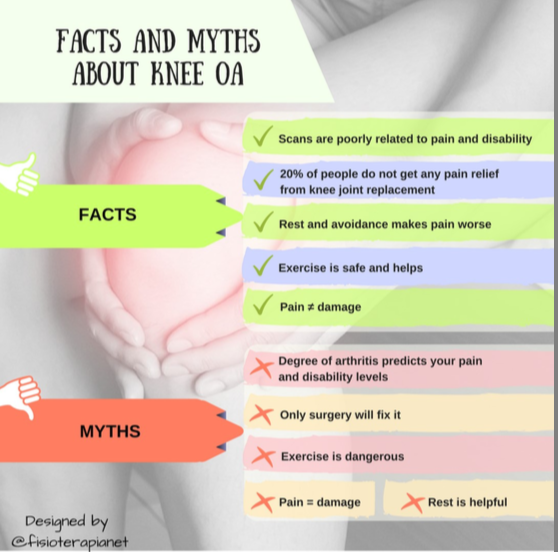
The old view of OA is that it a result of wear and tear and inevitable joint degeneration.
This is known as the biomedical model and it offers an overly simplistic view that OA happens when the cartilage in your knee joint starts to wear down, causing pain, stiffness, and all-around discomfort.
It's not exactly an inspiring way to view the problem.
New view of OA:
Thankfully some very smart researchers, clinicians and doctors have come together to provide an updated explanation for knee OA and this involves taking a broader view of knee OA as an integrated whole body problem - that involves inflammation, metabolic health, immune system, diet, nutrition and even things like our beliefs and knowledge.
“Clinical outcomes in OA are influenced by multiple factors, including pain sensitization, psychological distress, muscle strength, BMI, inflammation, disease severity, and comorbidities,39 which may ultimately limit the maximum improvement in pain and function”.https://acrjournals.onlinelibrary.wiley.com/doi/full/10.1002/acr.25313
Essentially we have updated our model from a simple mechanical system (body is a machine that needs fixing) to seeing the body as an ecosystem (capable of positive adaptive and growth given the optimal conditions) that is capable of regenerating given the optimal environmental conditions.
This new approach is no shortage of a revolution and paradigm shift in how we see the body and it’s potential for healing.
It opens the door to many treatment options that were previously not even considered until very recently.
Benefits of Running with Knee OA:
Believe it or not, running can actually have some perks for folks with knee OA:
Improved Joint Function: Running can help keep your knee joints flexible and moving smoothly, which is super important when you've got OA.
Strengthening Muscles: When you run, you're not just working out your legs – you're also giving those supporting muscles around your knees a good workout. It's like building a sturdy support system for your knees!
Weight Management: Running is a great way to burn calories and keep your weight in check. And when you're carrying around less weight, there's less stress on your knee joints.
Mood Boost: Ever heard of a runner's high? It's a real thing! Running releases feel-good hormones in your brain, which can help lift your mood and ease stress – definitely a win-win!
Considerations for Running with Knee OA:
Before you lace up those shoes and hit the pavement, here are a few things to keep in mind:
Talk to a Pro: It's always a good idea to chat with a healthcare pro before starting any new exercise routine, especially if you've got knee OA. They can give you the lowdown on whether running is safe for you.
Take It Slow: Start with a gentle jog or brisk walk, and gradually build up your speed and distance over time. Rome wasn't built in a day, and neither is a runner!
Shoe Game Strong: Invest in a good pair of running shoes with plenty of cushioning and support. Your knees will thank you!
Watch Your Form: Pay attention to your running technique – aim for a mid-foot strike, keep your posture upright, and try to land softly to reduce impact on your knees.
Mix It Up: Running is great, but it's not the only game in town! Mix in some strength training and flexibility exercises to give your knees a well-rounded workout.