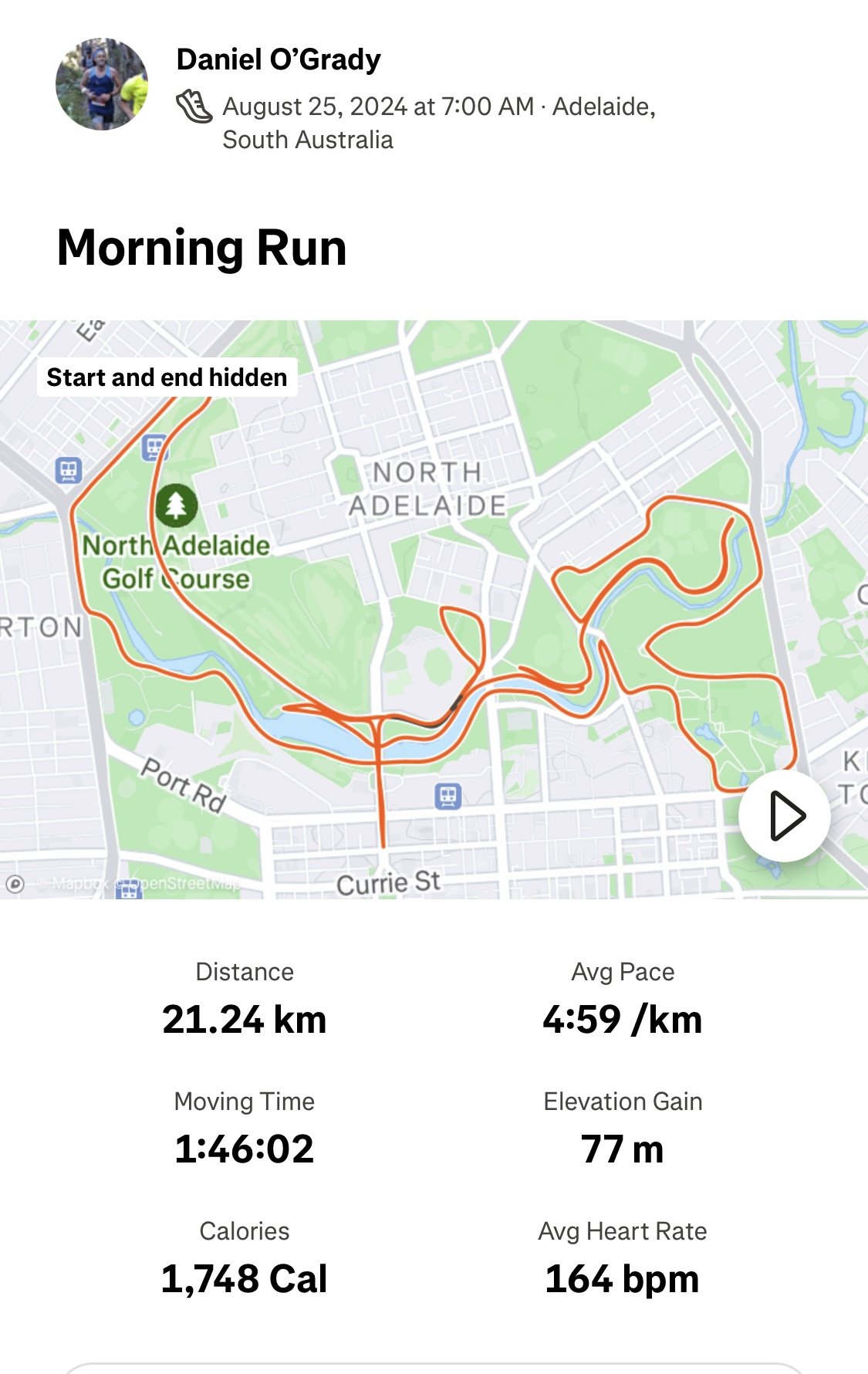
Adelaide, South Australia - 25th August 2024
This morning, I was looking for a bit of inspiration before lacing up for the Adelaide Half Marathon and happened to come across a short documentary on Robert de Castella’s iconic 1982 Rotterdam Marathon win.
Some of his words really stuck with me:
"You have to be prepared to push yourself through barriers of pain. The biggest pain you have to work yourself through is the incredible weariness, the incredible fatigue that envelops you like a cloud. You need to concentrate on achieving little goals. You can’t become totally introverted and withdrawn during the race, because you dwell on little things like how your feet are, losing a toenail or getting a blister, or sore muscles. You’ve got to monitor those things, but you can’t afford to let them become too dominant a feeling."
As the run started I could feel some great energy and buzz as we lined up outside of the Adelaide Oval.
For the past few years my goal has been to go under 1:45 for the half marathon and I have just missed out for less than a minute. My strategy has been to go out with the 1:45 pacing group from the start and try and hold on, but just seemed to be fatigue in the second half.
This year I thought I would change things up.
I decided to start with the 1:50 pacing group, with the idea being to relax for the first half running a little slower, save my energy and then come home really strong picking up the pace.
My run was going okay, but by the 17km mark, my legs were toast, with fatigue accumulating heavily after making some strong surges trying to pick up the pace.
I threw in a few walking breaks to try and get a bit of recovery.
Then, out of nowhere, I heard a voice from the sideline:
"C'mon, you've got this!"
I looked up, and there he was—the great man himself, Robert de Castella!
As if that wasn’t enough, I spotted a couple of very fit-looking Indigenous Marathon Project athletes just in front of me too.
That was the spark I needed to switch gears.
I found a new energy and finished the last 4km with a spring in my step, crossing the Morphett Street Bridge and finishing strong at Adelaide Oval.
My time - 1:46.
A huge thanks to SARRC and all the volunteers for making it a fantastic morning.
It was great to see everyone out there challenging themselves and running well!
I’m looking forward to getting back at there in 2025 - same goal - to break 1:45!