"We are all sculptors and painters. Our material is our own flesh, blood and bones." - Henry David Thoreau
This post takes a look at why we move the way we do, and how we can tap into the 'Power Of Plasticity' to start moving (and feeling) well again.
Warning: This post is long.
As the New Year ticks over, many of us find ourselves reflecting on our health and making some goals for the year ahead.
I can understand you may be reluctant to set a new years resolution.
But from the body’s view point, it desperately needs a goal to work towards.
It needs direction, positive growth, a challenge and a reason to get out of bed in the morning.
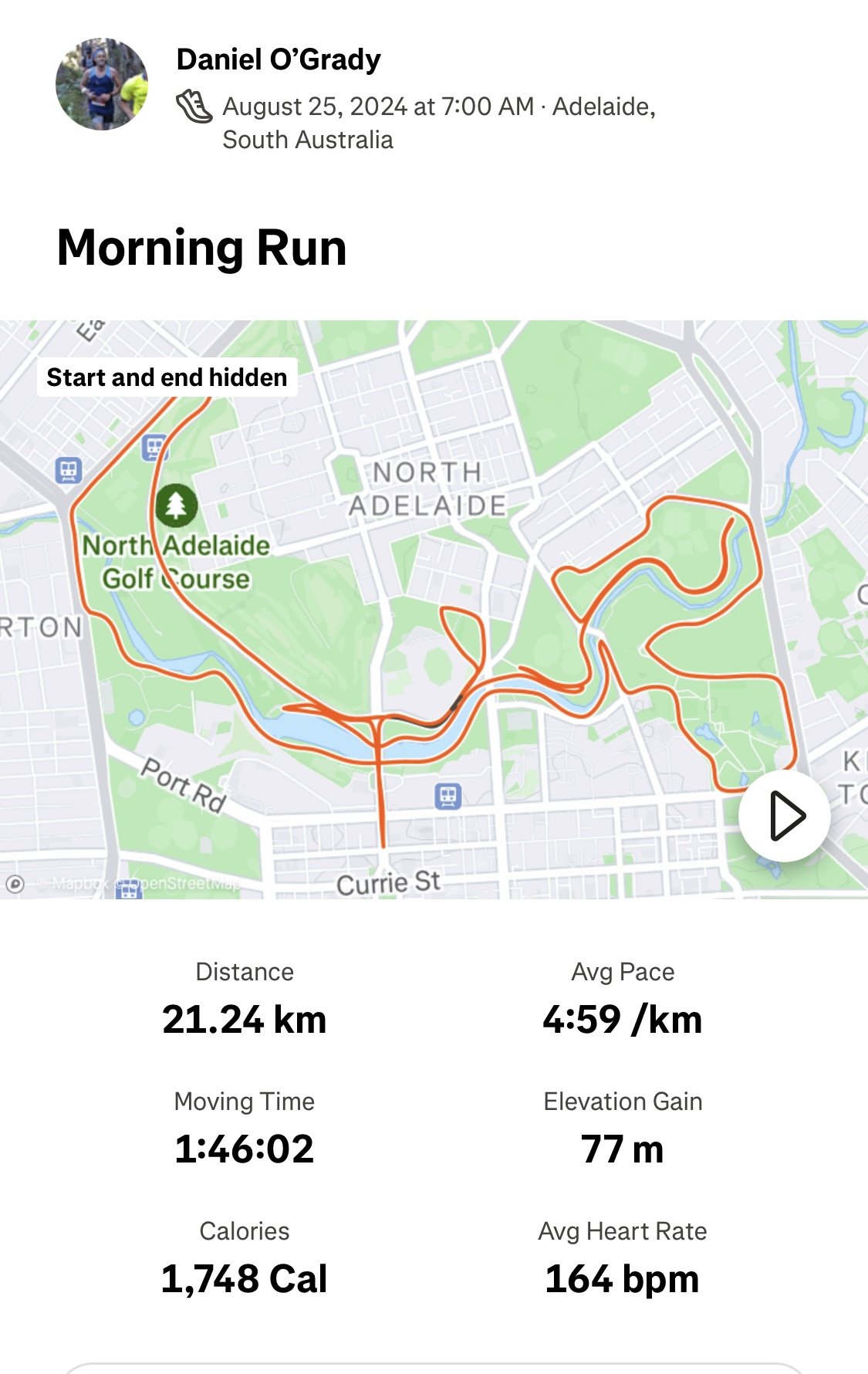
Your goal might be a run a marathon. Or it could be taking a challenging hike. Or spending the day in the garden.
Whatever it is, it should be something you enjoy and something that will motivate you to get you moving more often.
As soon as you become complacent about your body and your health, it can lead to a downward spiral of pain, injury and de-conditioning.
In modern day life with our attention being drawn into our devices, internet and netflix we can find ourselves completely out of touch with our bodies.
Months or years can easily slip by and all of a sudden we can find ourselves in a ‘movement rut’.
“Change is the only constant in life” - Heraclitus
Whether we are conscious of it or not, the body is always changing and adapting to the stresses we put it under.
From our bodies perspective you are either growing or stagnating.
There’s not much middle ground.
Plasticity: the adaptability of an organism to changes in its environment
That continual growth or stagnation that takes place is also known as plasticity.
As humans, we are highly adaptable and this can be a very positive thing.
The entire body is capable of plasticity
Professor Lorimer Mosely, from the University of South Australia, writes:
All our body systems respond to demand – in obvious ways such as:
growing muscle cells when we lift weights – myoplasticity
sweating more when we acclimatise – endoplasticity
learning to recognise a pathogen and eliminating it on next contact – immunoplasticity
increasing our heart-rate earlier on a hill after running up it a few times – cardioplasticity
adjusting the aperture of our pupil to improve our underwater vision – obiculoplasticity
the toughening of skin on well trodden heels – dermoplasticity.
In fact the body that you have today, is different is quite a bit different to the body you had a few days/weeks/years ago.
Regeneration Speeds Of The Human Body:
“The body is a powerful healing machine” - Kelly Starrett
These info-graphs refer to how our body parts are under a constant state of repair and regeneration (plasticity).
I’m not sure about you, but I find this knowledge really empowering and inspiring.
If you are in a difficult place right now, keep the faith and stick it out.
“Everything will be okay in the end. If it's not okay, it's not the end”. - John Lennon
With the right guidance and plan in place, good times are ahead for you.
If you can harness the power of positive plasticity you can get stronger, more resilient and eventually become pain-free.
Movement and Neuro-plasticity
This blog post is mainly focused on the neurological and muscular plasticity that happens in the body in response to movement.
We will take a look at how the healthy brain-body system operates when it’s fully “connected,” and conversely, what happens when things become dysfunctional.
Body Maps In The Brain
In many ways, our understanding of the brain has only just begun.
One of the most exciting developments in the 20th century was the identification of ‘body-maps’ in the brain.
The body maps refer to two of the principal areas in the brain involved in movement.
These include:
1. The Somato-Sensory Cortex - Encodes the representation of the entire body (i.e. body maps). Representational space correlates with how much a body part is used (i.e. use it or lose it)
2. The Motor Cortex - Generates conscious movement and stores subconscious movement patterns (i.e. muscle memory).
Our Body Maps Are Plastic
Neuroscience research suggests our brains are ‘plastic’ meaning that areas change depending on the amount and quality of use.
The more time and attention moving a certain body part, will result in a bigger representation of that area in the brain.
For example:
people who use braille have a larger finger representation in the brain than the average person
similarly guitar players will have a bigger hand representation in the brain
Body maps (and movement) comes to down to habits
Imagine you’re heading down to Aldinga for a day trip, (which is a beautiful beach an hours drive south of Adelaide, that allows cars onto the sand).
You arrive at the beach and follow the ramp down, driving your car onto the beach.
As you drive along the sand, your car makes tracks in the sand.
You find a nice spot to park the car and get yourself set-up. After you’ve had a swim, you’re feeling refreshed…but then you realise you’ve forgotten to buy some snacks.
So you jump back in the car and as you start driving, you can see the tracks you’ve made earlier.
As the sand is harder under the tracks, it’s easier for your car to move along the same tracks and reduce the likelihood of you getting bogged.
Each time you make a trip along the beach, the tracks get a little deeper and it gets a little easier to drive because the sand gets a little firmer and the track is becoming more worn.
You automatically keep using the same track without even thinking about it.
Using the same track is very similar to what happens with our bodies - the car represents our bodies movement and the tracks represent the neural pathways in our brain.
As our brains begin to use this pathway more, it becomes second nature.
This process of re-wiring the brain and forming new connections is plasticity in action.
Essentially using the same habitual movement patterns over and over again without ever thinking about it.
To create new movement patterns is like carving out a new road.
If you’ve had pain for some time, your body goes into protective mode. Movement expression becomes limited and breaking out of this stereo-typed response is going to take considerable energy, effort and some serious intent.
In an ideal world…
In an ideal world, the brain has a perfectly sharp representation of the body and the brain/body have a variety of quality movement patterns (muscle memory) to handle the demands placed on it.
The body and mind are perfectly synchronised.
An example of this might be watching Roger Federer playing tennis or Eddy Betts playing AFL.
They make highly complex skills look easy and effortless.
Body maps change when you’re in pain
Initially, when you’ve injured yourself or are in pain, the body map representation of the involved area actually gets bigger.
This explains why you may feel an increase in pain sensitivity and mild pains can become magnified.
This is especially true if the body part is very important to you e.g. if you injured your finger if you’re a concert pianist or your knee if you’re a runner.
The Negative Side Of Plasticity - Smudging
Smudging refers to the reduced accuracy of the body maps in the brain that happens when you don’t use a particular area for a period of time.
Smudging can be caused by things like:
poor posture
ongoing pain
injury
inactivity
More about brain smudging with David Butler:
Smudging of the brain maps, otherwise known as the Homunculus, latin for ‘little person’ in your brain
Credit: Explain Pain (Butler & Mosely)
“Pain and body image are closely related” – Norman Doidge
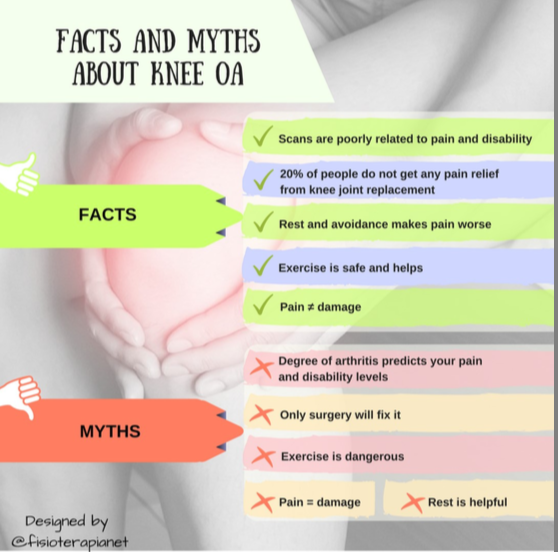
Studies have shown now that smudging of the body maps is related to the severity of lower back pain.
For example if you have injured your spine and you feel intense pain and muscle spasms for a few weeks, naturally, you may limit the amount of movement you will do for your spine.
Over time, there is less sensory input from the spine to the brain.
With limited input, the brain hasn’t got an accurate sense of what’s happening in the body (smudging of the body maps) and starts to perceives this as a threatening situation.
This is an important point because the pain you feel may not be related exclusively to a structural issue.
The fact is many people have degeneration / wear and tear and have absolutely no pain at all (see the chart below).
Pain, especially as it becomes more chronic, may be more related to changes in the nervous system (specifically the body maps in the brain).
The key point is that physical pain doesn’t necessarily have (only) physical causes.
Credit: Explain Pain (Butler & Mosely)
Key Point: A very large part of the way we move, comes to down the accuracy of our body maps
A large body of evidence shows that pain and injury causes a change in activity in the regions of our brains that control movement.
This is true for things like:
Everyone has their own unique response to pain and injury and I can’t emphasize enough the importance of getting a personalised movement assessment to find our your own individual patterning.
The first step is becoming aware, and then you can go about re-wiring your neural pathways and re-building your movement foundation.
If you aren’t consciously creating your movement patterns, you are in default mode - where your environment creates and dictates your movement.
Re-building Movement Patterns
“The more richer, the more varied the possibilities of your movement landscapes, the powerful you are” - Michael Merzencich
Back to our person with lower back pain example mentioned earlier.
Through pain and fear of doing more damage, their movement repertoire has become limited.
This results in:
A reduced ability to adapt to changes in their environment, leading to a higher chance of re-injury
Overload of tissues in the movement patterns that the person feels safe in e.g. they may have been told to always ‘sit up straight’ and the posterior back muscles are in a constant state of tension and activity
The original injury most likely has healed and the person now is dealing with the consequences of the changed movement patterns.
For optimal long term health, gradually adding variability to your movement and posture is a critical skill to learn.
In the world or ergonomics, having a variety of movements trumps locking into a narrow and restricted definition of ‘good posture’.
Creating the right conditions and environment to learn new movement patterns and strategies is what we’ll spend more time discussing this in Part 2 of this blog.
Key Take Home Messages:
The key to tapping into your bodies potential is neuro-plasticity, the process of creating new neural pathways
Understanding neuro-plasticity is the most revolutionary discovery of neuroscience in the past century.
There is great hope for people with chronic pain if you can access the power of movement neuro-plasticity
“The relationship between pain and the state of the tissues becomes weaker as pain persists” - D Lorimer Mosely
Widening our treatment approach to integrate the research on neuro-plasticity may be the missing link in helping people with chronic pain conditions
In Part 2 of the blog, we’ll go into depth about how to optimise your lifestyle to enhance and encourage the benefits of movement neuro-plasticity.