A new patient from last week prompted this post. He is a 43 year old presenting with persistent calf pain during running. ⠀⠀⠀⠀⠀⠀⠀
He's been a competitive cyclist most of his life. Now, as a father of three young ones he is attempting to make the transition from cycling to running. As his time is limited, he wanted a sport that maximizes his 'bang for buck'. ⠀⠀
⠀⠀⠀⠀⠀⠀⠀
He was frustrated because he generally felt very fit and never had any trouble with injuries as a cyclist.
⠀⠀⠀⠀⠀⠀⠀
On assessment, his calves and hamstrings were weak, hip flexors very tight, and gluteal muscle function poor. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀
⠀⠀⠀⠀⠀⠀⠀
Long story short, his strong lung capacity from cycling allowed him to push his body well past what it was prepared for and into the danger zone of overload and injury. ⠀
⠀⠀⠀⠀⠀⠀⠀
Tim Gabbett - "It's not the load that breaks the individual down. It's the load they are not prepared for."
⠀⠀⠀⠀⠀⠀⠀
A really common scenario & and probably explains why triathletes find themselves injured so often. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀
A research study (Rendos et al 2013) confirmed that cyclists develop muscle imbalances (particularly tight hip flexors) that can increase the risk of lower extremity injuries. ⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ ⠀⠀⠀⠀⠀⠀⠀
Key Points:
⠀⠀⠀⠀⠀⠀⠀
1. Cycling, while beneficial for cardio health can contribute to muscle balances that can set you up for an injury.
⠀⠀⠀⠀⠀⠀⠀
2. The human body is adaptable to change, but needs plenty of TIME to adapt. The fascia, muscles and tendons can take months/years to build capacity, while the cardio system responds much quicker. ⠀
⠀⠀⠀⠀⠀⠀⠀
3. Running is a high load activity & has the potential to cause long-term problems if you take on too much too soon. ⠀⠀⠀⠀⠀⠀⠀
4. An individualized Movement Assessment and corrective program will help maintain your body and keep it moving optimally. ⠀
⠀⠀⠀⠀⠀⠀⠀
The Resilient Runner Workshop takes the latest evidence-based research and practical strategies to optimize your movement foundation so that you not only avoid injury, but enhance your running performance.
Saturday June 2nd. 12pm - 3pm.
2 spots left. More details via this link
Tennis Elbow: Fast Track Your Healing
Tennis Elbow: 6 Steps To Fast Track Your Healing
Tennis elbow is a common condition experienced by many people.
It tends to affect people:
who use their arms a lot for work
most common between the ages of 35 and 50
people who have other conditions such as diabetes, high blood pressure, menopause
people who are very active, especially with a big competition goal coming up tend to push themselves to get fitter
Interestingly, only about 5% of people suffering from tennis elbow actually play tennis!
What is tennis elbow?
Tennis elbow refers to pain coming from the tendons of the forearm that join up to the elbow.
These tendons run from the fingers and wrist right up through the forearm and eventually insert into the elbow.
Symptoms of tennis elbow
Comes on gradually, related to a recent change in loading
Sore during warm up but feels better during activity
Often worst 24-48 hours after activity
Tendons can become inflamed when severe limiting movement
6 Steps To Fast Track Your Healing
Step 1. Get the right diagnosis first
You will need to have a thorough examination by a physiotherapist to determine if you have any referred pain from your neck and shoulder or if your elbow pain is isolated.
This will assist in a more direct approach to your problem and a speedier recovery.
Elbow pain can be coming from various sources such as:
Referred pain from your neck and shoulder can cause tennis elbow
Once you have been diagnosed with tennis elbow, it’s important to have realistic expectations of recovery.
Patience is definitely required as the healing process of tendons is longer than any other tissue in the body and take anywhere from 2 months to 2 years to full recover from tennis elbow.
You may need to continue with an exercise regime in the longer term - even after you stop seeing your physiotherapist.
This will ensure that your pain stays away for good.
Learning to listen to your body and know how much your arms can handle is a very important skill to learn as you recover.
Step 2. Calm things down
Generally we use two stage process for helping tennis elbow:
Calm things down
Build things back up
Calm things down:
Avoid aggravating activities and other things such as aggressive stretching
Stay calm and know that it will get better - your body is a powerful self healing machine
Write a list of all the activities that aggravate it (see below) and then prioritise the activities with the most important at the top. Try and cut out or delegate 80% of the activities that aren’t important for you to keep going
Cut the remaining load by 50% for 2 weeks and if you haven’t noticed a difference, you may need to cut the load more
Load = duration + intensity of an activity. If you can’t modify duration, you can modify intensity
Learn to listen to your body during an activity and the 24 hours after when the tendon will communicate with you
Common activities that increase the load on the elbow tendons are:
computer use - typing, using mouse e.t.c.
texting on your phone
gardening / weeding
Lifting heavy weights - bicep curls, overhead, swings, pullups
lifting groceries all in one go
carrying a heavy bag around
knitting
lifting small / big children
racquet sports or rowing
Push-ups / yoga / body weight exercise on arms
Massaging / manual therapy
playing musical instruments
ironing
doing dishes
peeling vegetables
gripping a bicycle handle or car steering wheel
Step 3. Ice/ Heat and TENS
Apply ice to the elbow regularly to reduce the pain and inflammation, particularly at the early onset of pain.
Some people find heat in the form of a wheat pack works better, as this can reduce the tension in the muscles and increase blood flow.
Another option is using a TENS machine that can stimulate blood flow to the muscles and tendons (this gives only short term relief and must be used in conjunction with other methods listed).
Step 4. Massage and dry needling
Techniques such as massage and dry needling can be used to release tension around the arms, shoulders and upper back.
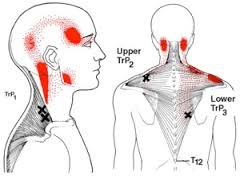
Muscles that have been overused over a long period of time often form knots or trigger points that can be palpated easily.
When tight, they can become a source of referred pain, with each muscle having a different area of referral (see below).
Dry needling has the ability to get achieve a quicker and more effective deep release of the muscles. As tendons have quite poor blood supply, dry needling can also stimulate the deep blood flow and increase the healing process.
The effects of Dry Needling were studied in this new study that took 110 people with tennis elbow and evaluated two treatments.
One group received dry needling and other group received anti-inflammatory medication (Ibuprofen 100mg x 2 day) and a brace.
The patients were evaluated after three weeks and six months.
Results:
Although both treatment methods were effective at three weeks, dry needling was significantly more effective than the medication and brace group at six months.
Conclusion:
Because of the low complication rate, dry needling is a safe method, and it might be a more effective treatment option for tennis elbow.
At Kinfolk Physio & Wellness, in addition to specialising in dry needling, we also take a holistic view of your movement and set you up with a personliased home exercise program that maintains flexibility and builds strength and capacity, to give the best long term solution.
If you would like to get your elbow pain on the fast track to healing, please click below to book an Initial Assessment (or call us 1300 657 813).
Step 5. Graduated loading program
At the end of the day, we want to gradually build the capacity of your forearm muscles so they can withstand the demands from your daily life.
This involves a graduated, progressive program of specific strengthening under the supervision of a Physiotherapist.
We follow a 12 weeks program to rebuild strength in the muscles of the forearm, shoulder and even through the neck and core muscles.
You would be doing exercises 2-3 x per week for about 15 minutes.
Tendons require gradual load in order to heal properly, so it’s very important to continue to strengthen your muscles even if your pain has improved.
To find out more about our loading program for tennis elbow and start your journey, please use our easy online booking system by clicking below.
Step 6. Create the optimal healing environment
With tendon problems, it’s really important to know that your body is always trying to heal itself.
So it’s important to try and create the optimal environment for that healing to take place.
This would include:
Get a good 7-8 hours of good quality sleep per night
Eat a high energy diet with sufficient protein and carbohydrates
Get enough rest during the week
Decrease stress in your life as much as possible
Ensuring your ergonomics at work are suitable
Do I need a cortisone injection?
If first-line treatments aren’t working a more invasive approach could be considered that includes a corticosteroid injection.
Corticosteroid injections, while giving effective short term relief, tend to wear off after 6-12 months, and the pain can return, (often worse than before).
The problem also with cortisone injections is they tend to weaken the tendons in the elbow, greatly increasing the risk of future overload.
Dan O'Grady is a results driven qualified Physiotherapist and member of the Australian Physiotherapy Association. Dan has a special interest in treating elbow pain. He has been working in private practice for 15 years. He is passionate about helping people to move better, feel better and get back to doing what they love.
How To Return To Running (Without Doing Another Injury)
The research is pretty clear that the biggest risk factor for an injury is a past injury.
Pain and injury can trigger off protective mechanisms that can sometimes be tricky to identify and overcome.
For many runners returning from an injury, a common theme is to run within yourself, intuitively trying to protect the body from further injury.
Top 10 Muscles That Respond To Dry Needling
Top 10 Muscles That Respond To Dry Needling
One of the benefits of dry needling is it's a very precise way of releasing a muscle.
Compared to massage, getting a twitch response out of a muscle gives a very predictable and effective release, deep from within the muscle belly.
In this post, I wanted to give you some insight into some of the best responding muscles that dry needling can help with.
If you want to learn more about exactly how dry needling works, please read more here.
Of course dry needling can be done to any muscle. The following post is to give you some insight into some commonly treated muscles that give especially good 'bang for your buck'.
*Please also see some important notes at the end of the post.
1. Deltoids
In terms of shoulder pain, the deltoid is a very under-rated muscle.
The deltoids include three sections (anterior, middle and posterior) that sit superficially around the shoulder. The deltoid is involved in almost all shoulder movement.
The way the it wraps around the shoulder makes it a very difficult muscle to stretch and it is prone to building up tension.
Trigger points and knots often develop in the deltoid that can give rise to shoulder pain (see pic above).
This pain can be quite severe and unrelenting and stubborn to usual treatment.
A common history is over-doing some push-ups and waking up the next day with pain in the front of the shoulder.
Or someone who has done a lot of heavy over-head weights (Cross fitters...!) over the years and doesn't do much stretching.
Sometimes it's the last small movement and final straw the breaks the camels back so to speak.
Dry needling the deltoid often gets some powerful twitch responses.
Expect soreness and a dead arm feeling for a few days before things settle down.
2. Latissimus Dorsi
The latissimus dorsi is a fascinating muscle.
It has attachments to the hip, shoulder, upper back, lower back and rib cage - and that makes it the largest muscle in the upper body.
Tightness in the latissimus dorsi has been shown to be an important cause of chronic shoulder pain and chronic back (especially upper back) pain.
Because of its extensive attachments, it can be another difficult muscle to stretch effectively.
Dry needling gets in there and gets the job done.
If your lats are tight, you will need to add in some regular childs pose and over-head stretching, in addition to foam rolling your upper back.
3. TFL / ITB
The fastest way to release your ITB ?
Release the under-rated small muscle that attaches to it, called the Tensor Fascia Latae (TFL).
The TFL is a small but powerful hip flexor and usually tight from excessively sitting, walking, running and cycling.
When overly tight, can contribute to knee pain by causing mis-tracking of the kneecap.
Combine dry needling with some specific gluteal activation and you will be well and truly on the way to saying goodbye to your ITB pain and tightness.
If you look after your TFL well, there's a good chance that excruiating ITB foam rolling will not be required. Happy days :-)
4. Glutes
One of the cool things about dry needling is that we can access deep points in a muscle that you would otherwise be unable to access.
The gluteus medius is an interesting muscle that can be dysfunctional in chronic lower back pain, hip pain and knee pain.
Dry needling can immediately 're-set' the glutes and allow for a graduated re-loading program.
Long-term, a well functioning gluteus medius will protect your hips, knees, ankles and lower back.
5. Calf - Gastrocnemius & Soleus
Calf muscle tension and limited flexibility is especially common in the modern age.
When tight, the calf muscles are prone to cramping and eventually tearing.
Deep tissue massage can be effective, but can be very painful, bordering on intolerable.
Dry needling to the calf muscles, whilst intense, is quicker and more effective in its release.
Expect some treatment soreness for 1-2 days post-needling.
And don't forget to re-build your calf capacity with an appropriate strengthening program.
6. Upper Trapezius
Much like the calf above, the upper traps can be loaded with tightness.
Causes can include poor posture, lack of physical activity and prolonged stress.
Heavy handed massage can stir up more irritation in the muscle.
Dry needling is more like using a sniper approach - with a few direct releases, you can release the traps and get the blood flowing much more effectively and deeply.
This study recommended dry needling for immediate pain reduction in upper body myofascial trigger point dysfunction.
Using heat on the traps via a wheat pack is really helpful, especially in the evening before bed.
Also make sure you are getting enough down time as chronic upper traps tension is a sign of sympathetic over-activity.
7. Infraspinatus
The infraspinatus is a sneaky little muscle that sits behind your shoulder blade.
It is often weak and gets overloaded when using your arm and shoulder.
When the infraspinatus gets tight, you'll often feel pain in the front and deep part of your shoulder.
Dry needling de-activates the trigger points quickly, but be prepared for a dead arm for a few hours.
Don't forget to re-build with some simple strengthening exercises with a thera-band.
8. Wrist Extensors
Tennis elbow is a very common condition that primarily affects the extensor tendons on the outside of the forearm.
The pain often drags on for months and years due to a very poor blood supply in the elbow tendons.
The research shows that dry needling releases a very specific chemical, known as Platelet-Derived Growth Factor (PDGF), that produces a strong increase in blood flow into the muscle.
In effect, blood is a healing agent, bringing oxygen and critical healing chemicals to the damaged cells.
No other technique that I know of is capable of doing this.
9. Biceps
When was the last time you stretched your bicep muscle?
Another muscle that gets used a lot, and builds up a great deal of tension.
You'd be surprised how that niggling pain in the front of your shoulder improves after your biceps is released through dry needling.
10. Hamstrings
Tight hamstrings are pretty common.
Stretching them normally does more harm than good (see here).
Dry needling produces a quick and effective release.
Specific strengthening exercises that lengthen the muscle gives the best long term solution.
Conclusion
Dry needling certainly isn't for everyone, but it can be a very effective and powerful treatment in the right context.
Two quick notes:
1. There are different types of dry needling and this blog refers to the type that activates a local twitch response.
This is very different to acupuncture and dry needling where the needles are inserted superficially and left in for 20 minutes as the practitioner leaves the room.
2. Dry needling is always used as part of comprehensive treatment approach.
This includes assessing your thoughts and beliefs about your injury, movement patterning and general health considerations.
Specific exercises targeted towards your individual needs will help give you the best long-term outcome.
If you have any questions about dry needling - please feel free to give us a call 1300 657 813.
If you'd like to schedule a dry needling session and start feeling better straight away, please book online below:
Gluteal Tendinopathy - How Physio Can Help
How do I know if I have gluteal tendinopathy?
The pain associated with gluteal tendinopathy is usually centred over the greater trochanter, the large bone that you can feel at the side of the hip, but may extend down the outer thigh towards the knee.
Pain may be felt when walking, particularly at speed, uphill or upstairs and when standing on one leg to dress.
It is common to experience pain and a feeling of stiffness when rising from a chair after prolonged sitting. Night time is often worse, particularly when lying on your side.
Your physiotherapist will take note of your history and symptoms and perform a number of physical tests in order to diagnose gluteal tendinopathy and rule out other potential sources of pain.
Radiological investigations such as an ultrasound scan or MRI may be used to confirm the diagnosis.
Many people without pain have tendon changes on scans, therefore clinical testing is required to determine whether scan findings are relevant to your current condition. It is not necessary to have scans before presenting to your physiotherapist for assistance. Most people can be diagnosed with clinical tests.
What causes gluteal tendinopathy?
Researchers are still working on clearly determining the causes of tendinopathy.
It is currently thought that the pain of gluteal tendinopathy often appears when the tendons become overloaded. This may be due to rapid increases in training or exercise load, a large force associated with a slip or fall or an increase in bodyweight.
Sometimes there has been no particular incident but there may have been a gradual weakening of the tendons over time associated with lack of stimulus of the gluteals due to low activity levels, or certain postural and movement habits.
Those with gluteal tendinopathy have been shown to have weakness in the gluteal muscles that attach to the problem tendons. If the muscles and their tendons become weak enough, they will fail to cope with everyday loads and your nervous system may warn you about this in the form of pain.
How can physiotherapy help with gluteal tendinopathy?
Physiotherapy can help in multiple ways. Your physiotherapist can advise you about controlling aggravating tendon loads—everyday postures, movement habits and activities that might be provoking your pain. Your physiotherapist can help to address poor postural and movement habits, including gait retraining.
Research has found that exercise provides the best long-term outcomes for tendon pain.
A specific exercise program that aims to improve your movement patterns, gradually strengthen the muscles involved and improve the health of your hip tendons is essential. Massage, self trigger point releases, acupuncture, dry needling and heat may assist with short term symptomatic pain relief.
However, a specific exercise program and being taught how to control loads across your tendons are key strategies in managing this condition for the longer term.
Stretching of the gluteals or Iliotibial band (ITB), while a common strategy, will usually only aggravate the tendons. Corticosteroid injections have previously been recommended, but these have been found to have only short term benefits. Surgery is reserved for cases that have not responded to any conservative treatments.
How effective is physiotherapy for gluteal tendinopathy?
There is currently a lack of evidence available from clinical trials for any interventions specifically designed for people with gluteal tendinopathy. Given this limited information, physiotherapists use information from other tendinopathy research, which shows that addressing the underlying causes of the tendinopathy and known strength deficits is the best way to manage tendinopathy.
What can I do at home?
Avoid stretching and rubbing firmly over the bone and avoid activities that worsen your pain. It is important to remember that complete rest does not heal tendon problems and the more inactive you become, the weaker you become.
Visiting your physiotherapist as soon as possible will help you to get on track with a tailored education and exercise program.
It’s best to avoid crossing your legs and when standing keep your weight over both legs evenly. Hanging off one hip in standing tends to compress the gluteal tendons and make the pain worse.
How long until I feel better?
With specific advice and a tailored exercise program, most people will notice some reduction in pain within 2-4 weeks. However, it will usually take a commitment to an exercise program over a number of months to regain adequate improvements in strength and movement patterns to consistently control symptoms and regain normal activity levels.
The time frame can vary significantly depending on the severity of the tendon problem, duration of the problem, previous interventions, level of muscle weakness or physical conditioning, other coexisting health problems and adherence with advice and exercise prescription.
Book A Free 20 Minute Discovery Session:
Includes:
- full injury history and movement assessment
- accurate diagnosis
- detailed treatment plan
*Valid for new patients only. Only 3 available per week.