The Resilient Knee Project is an innovative solution for people with chronic knee pain that empowers individuals to self-manage their pain and most importantly, get them back to enjoy the physical and mental benefits of running.
Founded by Daniel O’Grady, dedicated professional with first hand experience of overcoming knee pain and running the NYC Marathon, the project aims to be a world leader in restoring people’s confidence in their knees and get back to doing what they love.
Is The Resilient Knee Program right for you?
Take the free quiz here
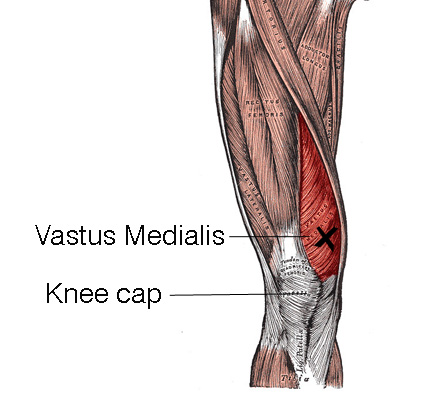
Get to your know your VMO
If you’ve ever had a nagging pain on the inside of your knee or a knee that seems to buckle or give way, there is a fair chance you’ve had some dysfunction in the VMO muscle.
VMO dysfunction is very common in runners, hikers, cyclists, athletes involved in jumping sports and after any knee injury.
In this short blog, we’ll find out more about how issues develop in the VMO and what you can do to help.
WHAT IS THE VMO MUSCLE?
VMO stands for Vastus Medialis Oblique and this is part of the quads, running along the inside of the thigh, with the bulk of the muscle sitting directly above the inside of the knee.
FUNCTION:
The role of the VMO is to assist with extending your knee and arguably the most responsible muscle for knee stability, as it helps control the alignment of the knee-cap.
When the VMO isn’t functionally optimally, the knee cap tends to shift slightly out of place during movements such as squats and lunges, causing pain and inflammation behind the knee-cap.
SYMPTOMS:
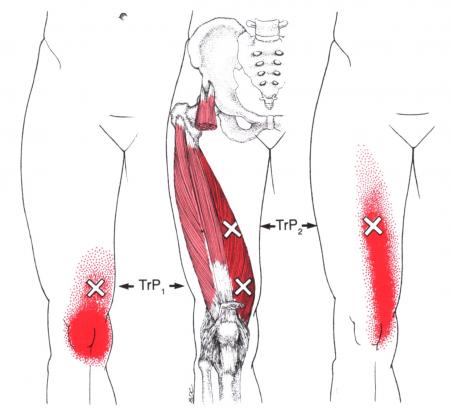
When the quads get overloaded (suddenly or over time), tightness in the muscle fibres (called trigger points) can refer a toothache-like pain deep in the knee joint (see Figure 1 below).
This pain from the overloaded VMO muscle can often be confused with joint pain such osteo-arthritis or a meniscus tear, as the location and type of pain are often similar.
Figure 1
The initial knee pain then may disappear after a few weeks, only to be replaced by a sudden weakness in the knee (a condition called “buckling knee”) that causes a person to unexpectedly fall while walking.
HOW THE VMO BECOMES OVERLOADED:
The VMO can be activated as a protective response to knee injury such as to the ligaments, meniscus or post-surgery.
The VMO is also commonly overloaded with repeated use in the following situations:
suddenly increasing your volume of running or cycling (running places around 6 x body weight through the quads)
a new (or sudden increase) in an exercise program involving repetitive squats, lunges, leg extensions or wall sits
jumping sports e.g. basketball
cycling - poor bike fit
walking downhill or stairs
being over-zealous in rehabbing the VMO - too much strengthening too soon
TREATMENT:
Physiotherapy assessment will involve a comprehensive movement assessment to determine the cause of your VMO issue.
“Short term treatment such as soft tissue massage and dry needling is very helpful, while long term building capacity in the quads, glutes and core is critical to prevent a relapse.
TRIGGER POINT DRY NEEDLING:
Tightness and contraction of the VMO responds very well to dry needling, which can de-activate the trigger points (knots in the muscle).
The benefit of dry needling is that it can reach the deep fibers of the muscle and lead to a quicker resolution of symptoms.
Treatment of the VMO is generally very responsive to treatment, provided the contributing factors are addressed.
SELF-CARE TIPS:
apply heat to the VMO muscle 10 minutes each day to increase blood flow and reduce tension
if you’re a runner or hiker, avoid the hills (in the short-term)
ensure your shoes are not overly worn
when running - avoid over-striding, ensure proper warm up and cool down and take walking breaks frequently to avoid overloading the VMO
avoid prolonged kneeling on the floor e.g. gardening, washing floors - use a low bench or stool to sit on instead
foam roll the VMO daily for a few minutes (see below). It’s also a good idea to roll out the adductors which are also commonly tight
Foam Roller for the VMO:
Foam rolling the inner quad and adductor - fun times!
Let’s get you back to doing what you love…
If you’d like to get your knee on the fast track straight away, please use the button below to schedule an appointment:
Dan O'Grady is a results driven qualified Physiotherapist and member of the Australian Physiotherapy Association. Dan has a special interest in treating knee pain. He has been working in private practice for 15 years. He is passionate about helping people to move better, feel better and get back to doing what they love.