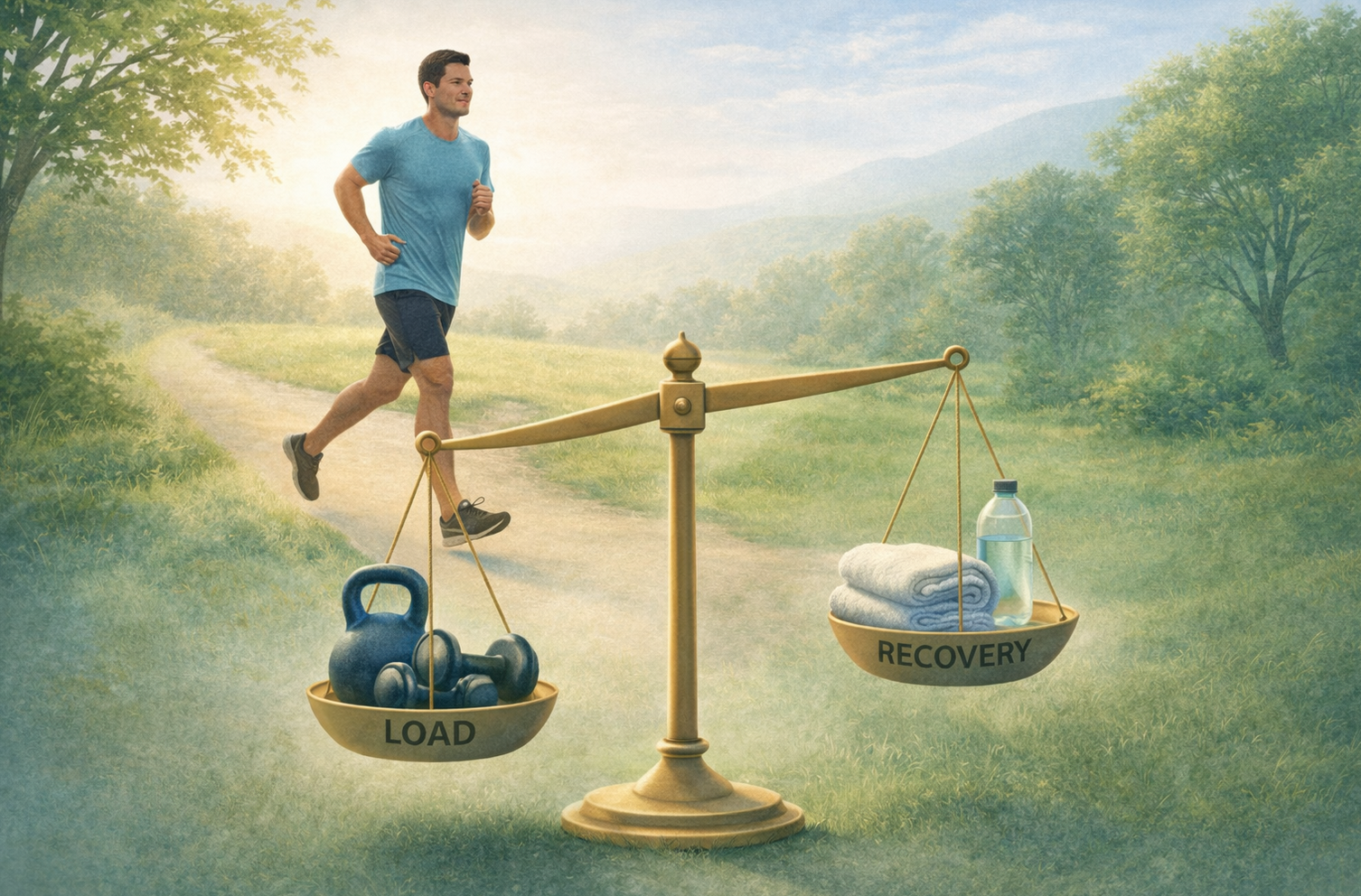
The only way to get better in the long term, is to gradually start building your physical capacity with a personalised program, so you can create a ‘zone of relaxation’ where you have the capacity to handle all of your daily life without the muscles becoming overloaded.
The trick is to build up gradually - step by step. As soon as you push too far you risk re-activating the tightness by over-loading the muscle.
In the beginning it is best to be conservative.
As your work with your body more, you will get to know and respect your bodies limits.
Some of the exercises you could include would be:
Acknowledging underlying emotional issues in chronic pain
When your neck symptoms are chronic, one of the most concerning things is the ongoing pain, which can sometimes go on for months or years, despite seeing multiple health care practitioners and trying different medications.
Understandably, this can create a lot of fear and anxiety about the underlying cause of the symptoms which can keep you in a state of fight or flight (see picture below).
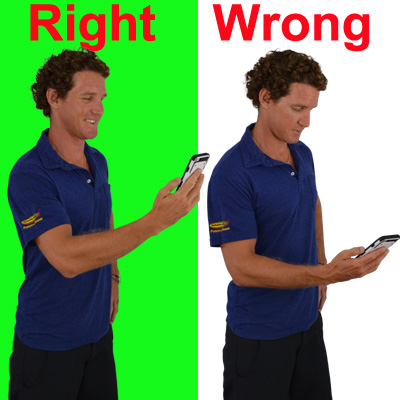
For some people, when they experience pain or injury it may be associated with anxiety and catastrophizing about the pain, like for example whether or not it will ever go away and if it will get worse if they move too much.
Some people become fearful of exercising and being active (known as ‘fear avoidance behaviour' and 'kinesiophobia') and might rely solely on passive treatment and resting, which can have some adverse effects and may lead to decreased function and a lower load threshold which could result in more pain.
As you can imagine, a downward spiral of fear, lack of movement, weakness and de-conditioning can result (see picture below) and become very difficult to break.
You are not your scan !
Often there have been some scans showing some damage to a structure such as a disc or nerve issue.
Injuries and structural issues certainly do cause pain initially.
Unfortunately, sometimes the patient is not given a broader context in which to interpret the significance of the results.
The body has a tremendous capacity to heal, and generally tissue damage takes no more than six to twelve months to occur.
If you are still getting pain after this time (and you have been thoroughly investigated by your health care team), your pain is more likely to be coming from a sensitized nervous system (see picture below) than an damaged structural fault.
One thing is very clear with the recent research is that you can have structural abnormality and have no pain whatsoever (see picture below).
Degeneration, disc issues and arthritis are very common in asymptomatic individuals (i.e. who have no pain - see picture below).
The ongoing nature of the pain is more often to do with tight muscles with restricted and oxygen blood flow.
Just understanding this process can go along way to resolving your ongoing pain issues, but you will need an experienced GP and Physio to work with to help you diagnose and get you back on the fast track.