If you've had a few niggles or been in pain recently, you might find yourself feeling a little overwhelmed. Sometimes the pain forces us into a defensive or protective mode.
Defensive strategies could include:
- ignoring the pain & hoping it will go away
- regularly taking pain killers / anti-inflammatory to numb the pain
- reducing or eliminating any sort of exercise for fear of causing a flare up
You may also find yourself bracing your body rigidly, every time you move or you may hold your breath (subconsciously) the majority of the time.
Defence IS an important short-term strategy for a new injury, don't get me wrong.
But, after a few months, you're tissues have generally healed the best they can.
Then you've got to take a leap of faith and breakout out of defence and start to re-build proactively...step by step.
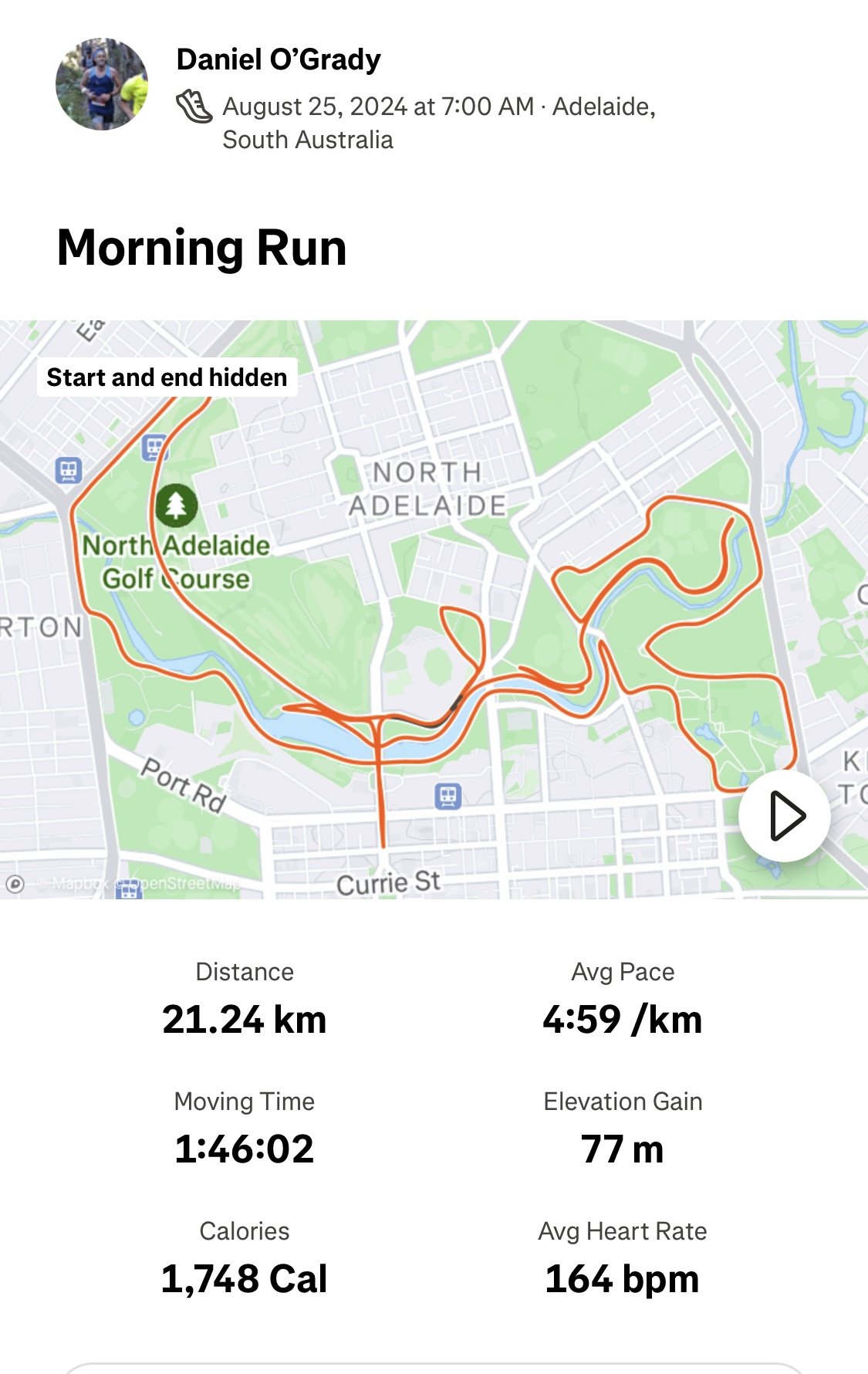
When planning your offensive play...success comes from having multiple strategies.
Just like in sport, if you're repeating the same offensive strategy all the time, your body will quickly see it coming and the positive adaptations become limited (and the risk of overuse injuries increases).
The best offence to build resilience in your body would include a good variety of types of movement.
Forming the foundation would be doing a form of Cardio aerobic exercise (whatever you enjoy), Pilates, Yoga, strengthening with a PT, and weight bearing exercise to stimulate bone growth.
Challenge for 2018:
Try x 5 NEW types of exercise or movement approaches that you haven't tried before.
TIP: try something that is the opposite of what you currently do. If you tend towards high intensity exercise than try something easier. If you tend to do easy stuff try something more intense.
Some movement options you could try:
- hiking, stand up paddle boarding, rock climbing, triathlon, cross fit, F45, orange theory fitness, Feldenkrais, karate, surfing, dancing, Parkour, BOUNCE, acroyoga, foam rolling, restorative Yoga, sprinting, 7 min workout, mountain biking, tennis, Aussie rules (especially for women!)
Keep challenging yourself.
Your body and mind will thank-you :-)